
Keratoconus
Encyclopedia
Keratoconus is a degenerative
disorder of the eye
in which structural changes within the cornea
cause it to thin and change to a more conical
shape than its normal gradual curve
.
Keratoconus can cause substantial distortion of vision
, with multiple images, streaking and sensitivity to light
all often reported by the patient. It is typically diagnosed in the patient's adolescent
years and attains its most severe state in the twenties and thirties. If afflicting both eyes, the deterioration in vision can affect the patient's ability to drive a car or read normal print. In most cases, corrective lens
es are effective enough to allow the patient to continue to drive legally and likewise function normally. Further progression of the disease may require surgery
including intrastromal corneal ring segments
, corneal collagen cross-linking, or corneal transplantation. However, despite the disease's unpredictable course, keratoconus can often be successfully managed with little or no impairment to the patient's quality of life
.
Keratoconus affects around one person in a thousand. It seems to occur in populations throughout the world, although it occurs more frequently in certain ethnic groups such as South Asians. The exact cause of keratoconus is uncertain, but has been associated with detrimental enzyme
activity within the cornea. Environmental and genetic factors are considered possible causes, but the findings are still yet inconclusive. The progression of keratoconus is rapid in patients having Down syndrome
.
 People with early keratoconus typically notice a minor blurring of their vision and come to their clinician seeking corrective lenses for reading or driving. At early stages, the symptom
People with early keratoconus typically notice a minor blurring of their vision and come to their clinician seeking corrective lenses for reading or driving. At early stages, the symptom
s of keratoconus may be no different from those of any other refractive defect
of the eye. As the disease progresses, vision deteriorates, sometimes rapidly. Visual acuity
becomes impaired at all distances, and night vision
is often quite poor. Some individuals have vision in one eye that is markedly worse than that in the other eye. The disease is often bilateral, though asymmetrical in many patients. Some develop photophobia
(sensitivity to bright light), eye strain from squinting in order to read, or itch
ing in the eye, but there is normally little or no sensation of pain
.
The classic symptom of keratoconus is the perception of multiple 'ghost' images, known as monocular polyopia. This effect is most clearly seen with a high contrast
field, such as a point of light on a dark background. Instead of seeing just one point, a person with keratoconus sees many images of the point, spread out in a chaotic pattern. This pattern does not typically change from day to day, but over time it often takes on new forms. Patients also commonly notice streaking and flaring
distortion around light sources. Some even notice the images moving relative to one another in time with their heart beat.
The predominant optical aberration of the eye as an optical system in keratoconus is the so-called coma
.
 Prior to any physical examination
Prior to any physical examination
, the diagnosis
of keratoconus frequently begins with an ophthalmologist's or optometrist's assessment of the patient's medical history
, particularly the chief complaint
and other visual symptoms, the presence of any history of ocular disease or injury which might affect vision, and the presence of any family history of ocular disease. An eye chart
, such as a standard Snellen chart
of progressively smaller letters
, is then used to determine the patient's visual acuity
. The eye examination
may proceed to measurement of the localised curvature of the cornea with a manual keratometer
, with detection of irregular astigmatism
suggesting a possibility of keratoconus. Severe cases can exceed the instrument's measuring ability. A further indication can be provided by retinoscopy
, in which a light beam is focused on the patient's retina
and the reflection, or reflex, observed as the examiner tilts the light source back and forth. Keratoconus is amongst the ophthalmic conditions that exhibit a scissor reflex action of two bands moving toward and away from each other like the blades of a pair of scissors
.
If keratoconus is suspected, the ophthalmologist or optometrist will search for other characteristic findings of the disease by means of slit lamp
examination of the cornea. An advanced case is usually readily apparent to the examiner, and can provide for an unambiguous diagnosis prior to more specialised testing. Under close examination, a ring of yellow-brown to olive-green pigmentation known as a Fleischer ring
can be observed in around half of keratoconic eyes. The Fleischer ring, caused by deposition of the iron oxide hemosiderin
within the corneal epithelium, is subtle and may not be readily detectable in all cases, but becomes more evident when viewed under a cobalt blue
filter. Similarly, around 50% of subjects exhibit Vogt's striae, fine stress lines within the cornea caused by stretching and thinning. The striae temporarily disappear while slight pressure is applied to the eyeball. A highly pronounced cone can create a V-shaped indentation in the lower eyelid
when the patient's gaze is directed downwards, known as Munson's sign
. Other clinical signs of keratoconus will normally have presented themselves long before Munson's sign becomes apparent, and so this finding, though a classic sign of the disease, tends not to be of primary diagnostic importance.
 A handheld keratoscope
A handheld keratoscope
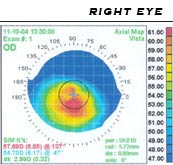
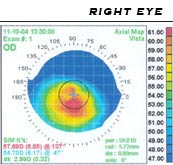
, sometimes known as Placido's disk, can provide a simple non-invasive visualization of the surface of the cornea by projecting a series of concentric rings of light onto the cornea. A more definitive diagnosis can be obtained using corneal topography
, in which an automated instrument projects the illuminated pattern onto the cornea and determines its topology from analysis of the digital image. The topographical map indicates any distortions or scarring in the cornea, with keratoconus revealed by a characteristic steepening of curvature which is usually below the centreline of the eye. The technique can record a snapshot of the degree and extent of the deformation as a benchmark for assessing its rate of progression. It is of particular value in detecting the disorder in its early stages when other signs have not yet presented.
Once keratoconus has been diagnosed, its degree may be classified by several metrics:
Increasing use of corneal topography has led to a decline in use of these terms.
of keratoconus remains unclear. Several sources suggest that keratoconus likely arises from a number of different factors: genetic, environmental or cellular, any of which may form the trigger for the onset of the disease.
in identical twins. The frequency of occurrence in close family members is not clearly defined, though it is known to be considerably higher than that in the general population, and studies have obtained estimates ranging between 6% and 19%. Two studies involving isolated, largely homogenetic communities have contrarily mapped putative gene locations to chromosome
s 16q and 20q. Most genetic studies agree on an autosomal dominant model of inheritance.
A rare, autosomal dominant form of severe keratoconus with anterior polar cataract is caused by a mutation in the seed region of mir-184
, a microRNA that is highly expressed in the cornea and anterior lens.
Keratoconus is diagnosed more often in people with Down syndrome
, though the reasons for this link have not yet been determined.
, allergies, and eczema
, and it is not uncommon for several or all of these diseases to affect one person. A number of studies suggest that vigorous eye rubbing contributes to the progression of keratoconus, and that patients should be discouraged from the practice. Iatrogenic
keratoconus has also been observed following LASIK
surgery, caused by removal of excessive stromal bed tissue.
 Once initiated, the disease normally develops by progressive dissolution of Bowman's layer, which lies between the corneal epithelium
Once initiated, the disease normally develops by progressive dissolution of Bowman's layer, which lies between the corneal epithelium
and stroma. As the two come into contact, cellular and structural changes in the cornea adversely affect its integrity and lead to the bulging and scarring that are characteristic of the disorder. Within any individual keratoconic cornea, there may be found regions of degenerative thinning coexisting with regions undergoing wound healing.
The visual distortion experienced by the patient comes from two sources, one being the irregular deformation of the surface of the cornea; the other being scarring that occurs on its exposed highpoints. These factors act to form regions on the cornea that map an image to different locations on the retina
and give rise to the symptom of monocular polyopia. The effect can worsen in low light conditions as the dark-adapted pupil
dilates to expose more of the irregular surface of the cornea. Scarring appears to be an aspect of the corneal degradation; however, a recent, large, multi-center study suggests that abrasion by contact lenses may increase the likelihood of this finding by a factor of over two. A number of patients complain of chronic eye rubbing and also think it as a possible cause to the disease but it is not so; however, it has been observed that keratoconus progresses faster due to eye-rubbing.
A number of studies have indicated that keratoconic corneas show signs of increased activity by protease
s, a class of enzyme
s that break some of the collagen
cross-linkages in the stroma, with a simultaneous reduced expression
of protease inhibitors
. Other studies have suggested that reduced activity by the enzyme aldehyde dehydrogenase
may be responsible for a build-up of free radicals and oxidising species in the cornea. It seems likely that, whatever the pathogenetical process
, the damage caused by activity within the cornea results in a reduction in its thickness and biomechanical strength. While keratoconus is considered a non-inflammatory disorder, one study shows that wearing rigid contact lenses by patients leads to overexpression of pro-inflammatory cytokine
s, such as IL-6
, TNF-alpha, ICAM-1
, and VCAM-1
in the tear fluid.
 In early stages of keratoconus, spectacles
In early stages of keratoconus, spectacles
or soft contact lenses can suffice to correct for the mild astigmatism. As the condition progresses, these may no longer provide the patient with a satisfactory degree of visual acuity, and most clinical practitioners will move to managing the condition with rigid contact lenses, known as rigid gas-permeables
, or RGPs. RGP lenses provide a good level of visual correction, but do not arrest progression of the condition.
In keratoconic patients, rigid contact lenses improve vision by means of tear fluid
filling the gap between the irregular corneal surface and the smooth regular inner surface of the lens, thereby creating the effect of a smoother cornea. Many specialized types of contact lenses have been developed for keratoconus, and affected people may seek out both doctors specialized in conditions of the cornea, and contact lens fitters who have experience managing patients with keratoconus. The irregular cone presents a challenge and the fitter will endeavour to produce a lens with the optimal contact, stability and steepness. Some trial-and-error fitting may prove necessary.
Traditionally, contact lenses for keratoconus have been the 'hard' or rigid gas-permeable variety, although manufacturers have also produced specialized 'soft' or hydrophilic lenses and, most recently, silicone hydrogel lenses. A soft lens has a tendency to conform to the conical shape of the cornea, thus diminishing its effect. To counter this, hybrid lenses have been developed which are hard in the centre and encompassed by a soft skirt. However, soft or earlier generation hybrid lenses did not prove effective for every patient. Early generation lenses like SoftPerm have been discontinued. The fourth generation of hybrid lens technology has improved significantly, giving more patients an option that combines the comfort of a soft lens with the visual acuity of an RGP lens. The new generation of technology fixes the issues that were prevalent in earlier generations and allows contact lenses to be fit for the majority of patients.
Some patients also find good vision correction and comfort with a "piggyback" lens combination, in which gas-permeable rigid lenses are worn over soft lenses, both providing a degree of vision correction. One form of piggyback lens makes use of a soft lens with a countersunk central area to accept the rigid lens. Fitting a piggyback lens combination requires experience on the part of the lens fitter, and tolerance on the part of the keratoconic patient.
Scleral lens
es are sometimes prescribed for cases of advanced or very irregular keratoconus; these lenses cover a greater proportion of the surface of the eye and hence can offer improved stability. The larger size of the lenses may make them unappealing or uncomfortable to some; however, their easier handling can find favour with patients with reduced dexterity, such as the elderly.
 Between 10% and 25% of cases of keratoconus will progress to a point where vision correction is no longer possible, thinning of the cornea becomes excessive, or scarring as a result of contact lens wear causes problems of its own, and a corneal transplantation or penetrating keratoplasty becomes required. Keratoconus is the most common grounds for conducting a penetrating keratoplasty, generally accounting for around a quarter of such procedures. The corneal transplant surgeon trephine
Between 10% and 25% of cases of keratoconus will progress to a point where vision correction is no longer possible, thinning of the cornea becomes excessive, or scarring as a result of contact lens wear causes problems of its own, and a corneal transplantation or penetrating keratoplasty becomes required. Keratoconus is the most common grounds for conducting a penetrating keratoplasty, generally accounting for around a quarter of such procedures. The corneal transplant surgeon trephine
s a lenticule of corneal tissue and then grafts
the donor
cornea to the existing eye tissue, usually using a combination of running and individual sutures. The cornea does not have a direct blood supply, and so donor tissue is not required to be blood type
matched. Eye bank
s check the donor corneas for any disease or cellular irregularities.
 The acute recovery period can take four to six weeks and full post-operative vision stabilization often takes a year or more but most transplants are very stable in the long term. The National Keratoconus Foundation reports that penetrating keratoplasty has the most successful outcome of all transplant procedures, and when performed for keratoconus in an otherwise healthy eye, its success rate can be 95% or greater. The sutures used usually dissolve over a period of three to five years but individual sutures can be removed during the healing process if they are causing irritation to the patient.
The acute recovery period can take four to six weeks and full post-operative vision stabilization often takes a year or more but most transplants are very stable in the long term. The National Keratoconus Foundation reports that penetrating keratoplasty has the most successful outcome of all transplant procedures, and when performed for keratoconus in an otherwise healthy eye, its success rate can be 95% or greater. The sutures used usually dissolve over a period of three to five years but individual sutures can be removed during the healing process if they are causing irritation to the patient.
In the USA, corneal transplants (also known as corneal grafts) for keratoconus are usually performed under sedation as outpatient surgery. In other countries, such as Australia and the UK, the operation is commonly performed with the patient undergoing a general anaesthetic. All cases require a careful follow-up with an eye surgeon (ophthalmologist) for a number of years. Frequently, vision is greatly improved after the surgery, but even if the actual visual acuity does not improve, because the cornea is a more normal shape after the healing is completed, patients can more easily be fitted with corrective lenses. Complications of corneal transplants are mostly related to vascularization of the corneal tissue and rejection
of the donor cornea. Vision loss
is very rare, though difficult-to-correct vision is possible. When rejection is severe, repeat transplants are often attempted, and are frequently successful. Keratoconus will not normally reoccur in the transplanted cornea; incidences of this have been observed, but are usually attributed to incomplete excision of the original cornea or inadequate screening of the donor tissue. The long-term outlook for corneal transplants performed for keratoconus is usually favorable once the initial healing period is completed and a few years have elapsed without problems.
before the incision is closed. The segments push out against the curvature of the cornea, flattening the peak of the cone and returning it to a more natural shape. The procedure, carried out on an outpatient basis under local anaesthesia, offers the benefit of being reversible and even potentially exchangeable as it involves no removal of eye tissue.
The principal intrastromal ring available is known by the trade name of Intacs. Internationally, Ferrara Rings are also available. Intacs are a patented technology and are placed outside the optical zone versus the smaller prismatic Ferrara rings that are placed just inside the 5 mm optical zone. Intacs are the only corneal implants that have gone through the FDA Phase I, II and III clinical trials and were first approved by the Food and Drug Administration
(FDA) in the United States in 1999 for myopia
; this was extended to the treatment of keratoconus in July 2004.
 Clinical studies on the effectiveness of intrastromal rings on keratoconus are in their early stages, and results have so far been generally encouraging, though they have yet to enter into wide acceptance with the refractive surgery community. In common with penetrating keratoplasty, the requirement for some vision correction in the form of spectacles or hydrophilic contact lenses may remain subsequent to the operation. Potential complications of intrastromal rings include accidental penetration through to the anterior chamber when forming the channel, post-operative infection
Clinical studies on the effectiveness of intrastromal rings on keratoconus are in their early stages, and results have so far been generally encouraging, though they have yet to enter into wide acceptance with the refractive surgery community. In common with penetrating keratoplasty, the requirement for some vision correction in the form of spectacles or hydrophilic contact lenses may remain subsequent to the operation. Potential complications of intrastromal rings include accidental penetration through to the anterior chamber when forming the channel, post-operative infection
of the cornea, and migration or extrusion of the segments. The rings offer a good chance of vision improvement even in otherwise hard to manage eyes, but results are not guaranteed and in a few cases may worsen.
Early studies on intrastromal corneal rings involved use of two segments to cause global flattening of the cornea. A later study reported that better results could be obtained for those cones located more to the periphery of the cornea by using a single Intacs segment. This leads to preferential flattening of the cone below, but also to steepening the over-flat upper part of the cornea.
solution is administered to the eye and is activated by illumination with UV-A light for approximately 30 minutes. The riboflavin causes new bonds to form across adjacent collagen strands in the stromal layer of the cornea, which recovers and preserves some of the cornea's mechanical strength. The corneal epithelial layer is generally removed in order to increase penetration of the riboflavin into the stroma.
Clinical trial
s are ongoing, but crosslinking is seeing increasing adoption by the ophthalmological community, and has shown success in retarding or stopping progression of the disease. Early results from an Australian study are very promising in reporting stabilization in all treated eyes, and a slight correction in visual acuity in most patients. The procedure, with epithelium removed, is approved for use throughout Europe, and commenced clinical trials in the USA in 2008. Over 300 patients have now been treated in the United States in those trials, which are composed of two randomized, controlled, multi-site clinical trials for the treatment of progressive keratoconus and post LASIK ectasia. Avedro Inc., the trial’s sponsor, is closing the follow-up phase of the study and completing the necessary steps to file the results with the FDA.
In some cases, collagen crosslinking may also be combined with other treatments to improve corneal asymmetry or optical refraction. Successful treatment methods include corneal ring segment inserts (INTACS or Ferrara Rings), Topography Guided Laser or Keraflex. Corrective lenses are normally required after these treatments but with smaller, more normalised prescriptions. Increased corneal symmetry allows for more comfortable contact lens wear, often of daily disposable lenses. These newer methods may have an important role in limiting deterioration of vision, increasing unaided/uncorrected vision and reducing the case for corneal transplantation.
procedure where the surgeon makes a spoke-like pattern of incisions into the cornea to modify its shape. This early surgical option for myopia
has been largely superseded by LASIK
and other similar procedures. LASIK itself is absolutely contraindicated in keratoconus and other corneal thinning conditions as removal of corneal stromal tissue will further damage an already thin and weak cornea.
For similar reasons, radial keratotomy has also generally not been used for keratoconic patients. However, an Italian clinic has reported some success with a modified asymmetric radial keratotomy procedure, in which the incisions are confined to one sector of the eye. The corneal thickness is first measured using a pachymeter
, then the surgeon makes cuts to a depth of 70–80% of the measured thickness. The patient may initially experience photophobia
and fluctuation of vision, in common with other forms of refractive surgery. This technique has yet to go through the official experimentation and follow-up period which is generally required by the Italian National Health Service to accept a new surgery technique before it can be offered to patients.
layer and the Descemet's membrane are left, giving some additional structural integrity to the post-graft cornea. Furthermore, it is possible to transplant tissue from a donor which has been freeze-dried
. The freeze-drying process ensures that this tissue is dead, so there is no chance of a rejection.
Some surgeons prefer to remove the donor epithelium, others leave the donor's cells in place. Removing it can cause a slight improvement in overall vision, but a corresponding increase in visual recovery time.
 Patients with keratoconus typically present initially with mild astigmatism
Patients with keratoconus typically present initially with mild astigmatism
and myopia, commonly at the onset of puberty
, and are diagnosed by the late teenage years or early 20s. The disease can however present or progress at any age: in rare cases keratoconus can present in children or not until later adulthood. A diagnosis of the disease at an early age may indicate a greater risk of severity in later life. Patients' vision will seem to fluctuate over a period of months, driving them to change lens prescriptions frequently, but as the condition worsens, contact lens
es are required in the majority of cases. The course of the disorder can be quite variable, with some patients remaining stable for years or indefinitely, while others progress rapidly or experience occasional exacerbations over a long and otherwise steady course. It tends to progress more rapidly in patients when the first presentation is in second decade of life. Most commonly, keratoconus progresses for a period of ten to twenty years before the course of the disease generally ceases in the third and fourth decades of life.
_due_to_keratoconus.jpg) In advanced cases, bulging of the cornea can result in a localized rupture of Descemet's membrane
In advanced cases, bulging of the cornea can result in a localized rupture of Descemet's membrane
, an inner layer of the cornea. Aqueous humor from the eye's anterior chamber
seeps into the cornea before Descemet's membrane reseals. The patient experiences pain and a sudden severe clouding of vision, with the cornea taking on a translucent milky-white appearance known as a corneal hydrops. Although disconcerting to the patient, the effect is normally temporary and after a period of six to eight weeks the cornea usually returns to its former transparency. The recovery can be aided non-surgically by bandaging with an osmotic
saline
solution. Although a hydrops usually causes increased scarring of the cornea, occasionally it will benefit a patient by creating a flatter cone, aiding the fitting of contact lenses. Occasionally, the cornea thins to the point that a partial rupture occurs at the level of Descemet´s membrane, resulting in a small, bead-like swelling on the cornea that may become filled with fluid (cornea hydropsy). When this occurs, severe vision decrease may occur until the edema slowly resolves. Corneal transplantation is not usually indicated while the hydropsy persists.
reports that keratoconus is the most common corneal dystrophy
in the United States, affecting approximately 1 in 2,000 Americans, but some reports place the figure as high as 1 in 500. The inconsistency may be due to variations in diagnostic criteria, with some cases of severe astigmatism interpreted as those of keratoconus, and vice versa. A long-term study found a mean incidence rate of 2.0 new cases per 100,000 population per year. It is suggested that males and females, and all ethnicities appear equally susceptible, though some recent studies have cast doubt upon this, suggesting a higher prevalence amongst females; the literature, however, varying as to its extent. Also, a study carried out in the UK suggests that people of a South Asian heritage are 4.4 times as likely to suffer from keratoconus as Caucasians, and are also more likely to be affected with the condition earlier.
Keratoconus is normally bilateral (affecting both eyes) although the distortion is usually asymmetric and is rarely completely identical in both corneas. Unilateral cases tend to be uncommon, and may in fact be very rare if a very mild condition in the better eye is simply below the limit of clinical detection. It is common for keratoconus to be diagnosed first in one eye and not until later in the other. As the condition then progresses in both eyes, the vision in the earlier-diagnosed eye will often persist to be poorer than that in its fellow.
 In a 1748 doctoral dissertation, the German oculist
In a 1748 doctoral dissertation, the German oculist
Burchard Mauchart
provided an early description of a case of keratoconus, which he called staphyloma diaphanum. However, it was not until 1854 that British physician John Nottingham clearly described keratoconus and distinguished it from other ectasia
s of the cornea. Nottingham reported the cases of "conical cornea" that had come to his attention, and described several classic features of the disease, including polyopia
, weakness of the cornea, and difficulty matching corrective lenses to the patient's vision. In 1859 British surgeon William Bowman used an ophthalmoscope (recently invented by Hermann von Helmholtz
) to diagnose keratoconus, and described how to angle the instrument's mirror so as to best see the conical shape of the cornea. Bowman also attempted to restore the vision by pulling on the iris
with a fine hook inserted through the cornea and stretching the pupil
into a vertical slit, like that of a cat. He reported that he had had a measure of success with the technique, restoring vision to an 18-year old woman who had previously been unable to count fingers at a distance of 8 inches (20 cm). By 1869, when the pioneering Swiss ophthalmologist Johann Horner wrote a thesis entitled On the treatment of keratoconus, the disorder had acquired its current name. The treatment at that time, endorsed by the leading German ophthalmologist Albrecht von Graefe, was an attempt to physically reshape the cornea by chemical cauterization with a silver nitrate
solution and application of a miosis
-causing agent with a pressure dressing. In 1888 the treatment of keratoconus became one of the first practical applications of the then newly invented contact lens
, when the French physician Eugène Kalt
manufactured a glass scleral shell which improved vision by compressing the cornea into a more regular shape. Since the start of the twentieth century, research on keratoconus has both improved understanding of the disease and greatly expanded the range of treatment options. The first successful transplantation of cornea to treat keratoconus was done in 1936 by Ramon Castroviejo
.
Keratoglobus
Pellucid Marginal Degeneration
Posterior keratoconus
Degenerative disease
A degenerative disease, also called neurodegenerative disease, is a disease in which the function or structure of the affected tissues or organs will progressively deteriorate over time, whether due to normal bodily wear or lifestyle choices such as exercise or eating habits...
disorder of the eye
Human eye
The human eye is an organ which reacts to light for several purposes. As a conscious sense organ, the eye allows vision. Rod and cone cells in the retina allow conscious light perception and vision including color differentiation and the perception of depth...
in which structural changes within the cornea
Cornea
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Together with the lens, the cornea refracts light, with the cornea accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is...
cause it to thin and change to a more conical
Cone (geometry)
A cone is an n-dimensional geometric shape that tapers smoothly from a base to a point called the apex or vertex. Formally, it is the solid figure formed by the locus of all straight line segments that join the apex to the base...
shape than its normal gradual curve
Curve
In mathematics, a curve is, generally speaking, an object similar to a line but which is not required to be straight...
.
Keratoconus can cause substantial distortion of vision
Visual perception
Visual perception is the ability to interpret information and surroundings from the effects of visible light reaching the eye. The resulting perception is also known as eyesight, sight, or vision...
, with multiple images, streaking and sensitivity to light
Photophobia
Photophobia is a symptom of abnormal intolerance to visual perception of light. As a medical symptom photophobia is not a morbid fear or phobia, but an experience of discomfort or pain to the eyes due to light exposure or by presence of actual physical photosensitivity of the eyes, though the term...
all often reported by the patient. It is typically diagnosed in the patient's adolescent
Adolescence
Adolescence is a transitional stage of physical and mental human development generally occurring between puberty and legal adulthood , but largely characterized as beginning and ending with the teenage stage...
years and attains its most severe state in the twenties and thirties. If afflicting both eyes, the deterioration in vision can affect the patient's ability to drive a car or read normal print. In most cases, corrective lens
Corrective lens
A corrective lens is a lens worn in front of the eye, mainly used to treat myopia, hyperopia, astigmatism, and presbyopia. Glasses or "spectacles" are worn on the face a short distance in front of the eye. Contact lenses are worn directly on the surface of the eye...
es are effective enough to allow the patient to continue to drive legally and likewise function normally. Further progression of the disease may require surgery
Surgery
Surgery is an ancient medical specialty that uses operative manual and instrumental techniques on a patient to investigate and/or treat a pathological condition such as disease or injury, or to help improve bodily function or appearance.An act of performing surgery may be called a surgical...
including intrastromal corneal ring segments
Intrastromal corneal ring segments
Intrastromal corneal rings are small devices implanted in the eye to correct vision. A typical vision correction using corneal rings would involve an ophthalmologist making a small incision in the cornea of the eye, and inserting two crescent or semi-circular shaped ring segments between the...
, corneal collagen cross-linking, or corneal transplantation. However, despite the disease's unpredictable course, keratoconus can often be successfully managed with little or no impairment to the patient's quality of life
Quality of life
The term quality of life is used to evaluate the general well-being of individuals and societies. The term is used in a wide range of contexts, including the fields of international development, healthcare, and politics. Quality of life should not be confused with the concept of standard of...
.
Keratoconus affects around one person in a thousand. It seems to occur in populations throughout the world, although it occurs more frequently in certain ethnic groups such as South Asians. The exact cause of keratoconus is uncertain, but has been associated with detrimental enzyme
Enzyme
Enzymes are proteins that catalyze chemical reactions. In enzymatic reactions, the molecules at the beginning of the process, called substrates, are converted into different molecules, called products. Almost all chemical reactions in a biological cell need enzymes in order to occur at rates...
activity within the cornea. Environmental and genetic factors are considered possible causes, but the findings are still yet inconclusive. The progression of keratoconus is rapid in patients having Down syndrome
Down syndrome
Down syndrome, or Down's syndrome, trisomy 21, is a chromosomal condition caused by the presence of all or part of an extra 21st chromosome. It is named after John Langdon Down, the British physician who described the syndrome in 1866. The condition was clinically described earlier in the 19th...
.
Signs and symptoms

Symptom
A symptom is a departure from normal function or feeling which is noticed by a patient, indicating the presence of disease or abnormality...
s of keratoconus may be no different from those of any other refractive defect
Refractive error
A refractive error, or refraction error, is an error in the focusing of light by the eye and a frequent reason for reduced visual acuity.-Classification:...
of the eye. As the disease progresses, vision deteriorates, sometimes rapidly. Visual acuity
Visual acuity
Visual acuity is acuteness or clearness of vision, which is dependent on the sharpness of the retinal focus within the eye and the sensitivity of the interpretative faculty of the brain....
becomes impaired at all distances, and night vision
Night vision
Night vision is the ability to see in low light conditions. Whether by biological or technological means, night vision is made possible by a combination of two approaches: sufficient spectral range, and sufficient intensity range...
is often quite poor. Some individuals have vision in one eye that is markedly worse than that in the other eye. The disease is often bilateral, though asymmetrical in many patients. Some develop photophobia
Photophobia
Photophobia is a symptom of abnormal intolerance to visual perception of light. As a medical symptom photophobia is not a morbid fear or phobia, but an experience of discomfort or pain to the eyes due to light exposure or by presence of actual physical photosensitivity of the eyes, though the term...
(sensitivity to bright light), eye strain from squinting in order to read, or itch
Itch
Itch is a sensation that causes the desire or reflex to scratch. Itch has resisted many attempts to classify it as any one type of sensory experience. Modern science has shown that itch has many similarities to pain, and while both are unpleasant sensory experiences, their behavioral response...
ing in the eye, but there is normally little or no sensation of pain
Pain
Pain is an unpleasant sensation often caused by intense or damaging stimuli such as stubbing a toe, burning a finger, putting iodine on a cut, and bumping the "funny bone."...
.
The classic symptom of keratoconus is the perception of multiple 'ghost' images, known as monocular polyopia. This effect is most clearly seen with a high contrast
Contrast (vision)
Contrast is the difference in visual properties that makes an object distinguishable from other objects and the background. In visual perception of the real world, contrast is determined by the difference in the color and brightness of the object and other objects within the same field of view...
field, such as a point of light on a dark background. Instead of seeing just one point, a person with keratoconus sees many images of the point, spread out in a chaotic pattern. This pattern does not typically change from day to day, but over time it often takes on new forms. Patients also commonly notice streaking and flaring
Lens flare
Lens flare is the light scattered in lens systems through generally unwanted image formation mechanisms, such as internal reflection and scattering from material inhomogeneities in the lens. These mechanisms differ from the intended image formation mechanism that depends on refraction of the image...
distortion around light sources. Some even notice the images moving relative to one another in time with their heart beat.
The predominant optical aberration of the eye as an optical system in keratoconus is the so-called coma
Coma (optics)
In optics , the coma in an optical system refers to aberration inherent to certain optical designs or due to imperfection in the lens or other components which results in off-axis point sources such as stars appearing distorted, appearing to have a tail like a comet...
.
Diagnosis

Physical examination
Physical examination or clinical examination is the process by which a doctor investigates the body of a patient for signs of disease. It generally follows the taking of the medical history — an account of the symptoms as experienced by the patient...
, the diagnosis
Medical diagnosis
Medical diagnosis refers both to the process of attempting to determine or identify a possible disease or disorder , and to the opinion reached by this process...
of keratoconus frequently begins with an ophthalmologist's or optometrist's assessment of the patient's medical history
Medical history
The medical history or anamnesis of a patient is information gained by a physician by asking specific questions, either of the patient or of other people who know the person and can give suitable information , with the aim of obtaining information useful in formulating a diagnosis and providing...
, particularly the chief complaint
Chief complaint
The Chief Complaint formally known as CC in the medical field, or termed Presenting Complaint in the UK, is a concise statement describing the symptom, problem, condition, diagnosis, physician recommended return, or other factor that is the reason for a medicalencounter...
and other visual symptoms, the presence of any history of ocular disease or injury which might affect vision, and the presence of any family history of ocular disease. An eye chart
Eye chart
An eye chart is a chart used to measure visual acuity. Types of eye charts include the logMAR chart, Snellen chart, Landolt C, and the Lea test.-Procedure:Charts usually display several rows of optotypes , each row in a different size...
, such as a standard Snellen chart
Snellen chart
A Snellen chart is an eye chart used by eye care professionals and others to measure visual acuity. Snellen charts are named after the Dutch ophthalmologist Herman Snellen who developed the chart during 1862...
of progressively smaller letters
Optotype
An optotype is a standardized symbol for testing vision. Optotypes can be specially shaped letters, numbers, or geometric symbols. For instance, to determine visual acuity, optotypes of different sizes are presented to a person and the smallest size is determined at which the person can reliably...
, is then used to determine the patient's visual acuity
Visual acuity
Visual acuity is acuteness or clearness of vision, which is dependent on the sharpness of the retinal focus within the eye and the sensitivity of the interpretative faculty of the brain....
. The eye examination
Eye examination
An eye examination is a battery of tests performed by an ophthalmologist, optometrist, or orthoptist assessing vision and ability to focus on and discern objects, as well as other tests and examinations pertaining to the eyes....
may proceed to measurement of the localised curvature of the cornea with a manual keratometer
Keratometer
A keratometer, also known as a ophthalmometer, is a diagnostic instrument for measuring the curvature of the anterior surface of the cornea, particularly for assessing the extent and axis of astigmatism...
, with detection of irregular astigmatism
Astigmatism (eye)
Astigmatism is an optical defect in which vision is blurred due to the inability of the optics of the eye to focus a point object into a sharp focused image on the retina. This may be due to an irregular or toric curvature of the cornea or lens. There are two types of astigmatism: regular and...
suggesting a possibility of keratoconus. Severe cases can exceed the instrument's measuring ability. A further indication can be provided by retinoscopy
Retinoscopy
Retinoscopy is a technique to obtain an objective measurement of the refractive error of a patient's eyes. The examiner uses a retinoscope to shine light into the patient's eye and observes the reflection off the patient's retina...
, in which a light beam is focused on the patient's retina
Retina
The vertebrate retina is a light-sensitive tissue lining the inner surface of the eye. The optics of the eye create an image of the visual world on the retina, which serves much the same function as the film in a camera. Light striking the retina initiates a cascade of chemical and electrical...
and the reflection, or reflex, observed as the examiner tilts the light source back and forth. Keratoconus is amongst the ophthalmic conditions that exhibit a scissor reflex action of two bands moving toward and away from each other like the blades of a pair of scissors
Scissors
Scissors are hand-operated cutting instruments. They consist of a pair of metal blades pivoted so that the sharpened edges slide against each other when the handles opposite to the pivot are closed. Scissors are used for cutting various thin materials, such as paper, cardboard, metal foil, thin...
.
If keratoconus is suspected, the ophthalmologist or optometrist will search for other characteristic findings of the disease by means of slit lamp
Slit lamp
The slit lamp is an instrument consisting of a high-intensity light source that can be focused to shine a thin sheet of light into the eye. It is used in conjunction with a biomicroscope...
examination of the cornea. An advanced case is usually readily apparent to the examiner, and can provide for an unambiguous diagnosis prior to more specialised testing. Under close examination, a ring of yellow-brown to olive-green pigmentation known as a Fleischer ring
Fleischer ring
Fleischer rings are pigmented rings in the peripheral cornea, resulting from iron deposition in basal epithelial cells, in the form of hemosiderin...
can be observed in around half of keratoconic eyes. The Fleischer ring, caused by deposition of the iron oxide hemosiderin
Hemosiderin
thumb|Hemosiderin image of a kidney viewed under a microscope. The brown areas represent hemosiderinHemosiderin or haemosiderin is an iron-storage complex. It is always found within cells and appears to be a complex of ferritin, denatured ferritin and other material...
within the corneal epithelium, is subtle and may not be readily detectable in all cases, but becomes more evident when viewed under a cobalt blue
Cobalt blue
Cobalt blue is a cool, slightly desaturated blue color, historically made using cobalt salts of alumina. It is used in certain ceramics and painting; the different cobalt pigment smalt, based on silica, is more often used directly in tinted transparent glasses...
filter. Similarly, around 50% of subjects exhibit Vogt's striae, fine stress lines within the cornea caused by stretching and thinning. The striae temporarily disappear while slight pressure is applied to the eyeball. A highly pronounced cone can create a V-shaped indentation in the lower eyelid
Eyelid
An eyelid is a thin fold of skin that covers and protects an eye. With the exception of the prepuce and the labia minora, it has the thinnest skin of the whole body. The levator palpebrae superioris muscle retracts the eyelid to "open" the eye. This can be either voluntarily or involuntarily...
when the patient's gaze is directed downwards, known as Munson's sign
Munson's sign
Munson's sign is a V-shaped indentation observed in the lower eyelid when the patient's gaze is directed downwards. The medical sign is characteristic of advanced cases of keratoconus and is caused by the cone-shaped cornea pressing down into the eyelid. It is named after American ophthalmologist...
. Other clinical signs of keratoconus will normally have presented themselves long before Munson's sign becomes apparent, and so this finding, though a classic sign of the disease, tends not to be of primary diagnostic importance.
Keratoscope
A keratoscope, sometimes known as Placido's disk, is an ophthalmic instrument for assessing the shape of the anterior surface of the cornea. A series of concentric rings are projected onto the cornea and their reflection viewed by the examiner through a small hole in the centre of the disk. A...
, sometimes known as Placido's disk, can provide a simple non-invasive visualization of the surface of the cornea by projecting a series of concentric rings of light onto the cornea. A more definitive diagnosis can be obtained using corneal topography
Corneal topography
Corneal topography, also known as photokeratoscopy or videokeratography, is a non-invasive medical imaging technique for mapping the surface curvature of the cornea, the outer structure of the eye...
, in which an automated instrument projects the illuminated pattern onto the cornea and determines its topology from analysis of the digital image. The topographical map indicates any distortions or scarring in the cornea, with keratoconus revealed by a characteristic steepening of curvature which is usually below the centreline of the eye. The technique can record a snapshot of the degree and extent of the deformation as a benchmark for assessing its rate of progression. It is of particular value in detecting the disorder in its early stages when other signs have not yet presented.
Once keratoconus has been diagnosed, its degree may be classified by several metrics:
- The steepness of greatest curvature from mild (< 45 DDioptreA dioptre, or diopter, is a unit of measurement of the optical power of a lens or curved mirror, which is equal to the reciprocal of the focal length measured in metres . It is thus a unit of reciprocal length. For example, a 3-dioptre lens brings parallel rays of light to focus at metre...
), advanced (up to 52 DDioptreA dioptre, or diopter, is a unit of measurement of the optical power of a lens or curved mirror, which is equal to the reciprocal of the focal length measured in metres . It is thus a unit of reciprocal length. For example, a 3-dioptre lens brings parallel rays of light to focus at metre...
) or severe (> 52 DDioptreA dioptre, or diopter, is a unit of measurement of the optical power of a lens or curved mirror, which is equal to the reciprocal of the focal length measured in metres . It is thus a unit of reciprocal length. For example, a 3-dioptre lens brings parallel rays of light to focus at metre...
); - The morphology of the cone: nipple (small: 5 mm and near-central), oval (larger, below-center and often sagging), or globus (more than 75% of cornea affected);
- The corneal thickness from mild (> 506 μm) to advanced (< 446 μm).
Increasing use of corneal topography has led to a decline in use of these terms.
Cause
Despite considerable research, the etiologyEtiology
Etiology is the study of causation, or origination. The word is derived from the Greek , aitiologia, "giving a reason for" ....
of keratoconus remains unclear. Several sources suggest that keratoconus likely arises from a number of different factors: genetic, environmental or cellular, any of which may form the trigger for the onset of the disease.
Genetic Causes
A genetic predisposition to keratoconus has been observed, with the disease running in certain families, and incidences reported of concordanceConcordance (genetics)
Concordance as used in genetics usually means the presence of the same trait in both members of a pair of twins. However, the strict definition is the probability that a pair of individuals will both have a certain characteristic, given that one of the pair has the characteristic. For example,...
in identical twins. The frequency of occurrence in close family members is not clearly defined, though it is known to be considerably higher than that in the general population, and studies have obtained estimates ranging between 6% and 19%. Two studies involving isolated, largely homogenetic communities have contrarily mapped putative gene locations to chromosome
Chromosome
A chromosome is an organized structure of DNA and protein found in cells. It is a single piece of coiled DNA containing many genes, regulatory elements and other nucleotide sequences. Chromosomes also contain DNA-bound proteins, which serve to package the DNA and control its functions.Chromosomes...
s 16q and 20q. Most genetic studies agree on an autosomal dominant model of inheritance.
A rare, autosomal dominant form of severe keratoconus with anterior polar cataract is caused by a mutation in the seed region of mir-184
Mir-184
In molecular biology, miR-184 microRNA is a short non-coding RNA molecule. MicroRNAs function as posttranscriptional regulators of expression levels of other genes by several mechanisms...
, a microRNA that is highly expressed in the cornea and anterior lens.
Keratoconus is diagnosed more often in people with Down syndrome
Down syndrome
Down syndrome, or Down's syndrome, trisomy 21, is a chromosomal condition caused by the presence of all or part of an extra 21st chromosome. It is named after John Langdon Down, the British physician who described the syndrome in 1866. The condition was clinically described earlier in the 19th...
, though the reasons for this link have not yet been determined.
Environmental Causes
Keratoconus has been associated with atopic diseases, which include asthmaAsthma
Asthma is the common chronic inflammatory disease of the airways characterized by variable and recurring symptoms, reversible airflow obstruction, and bronchospasm. Symptoms include wheezing, coughing, chest tightness, and shortness of breath...
, allergies, and eczema
Eczema
Eczema is a form of dermatitis, or inflammation of the epidermis . In England, an estimated 5.7 million or about one in every nine people have been diagnosed with the disease by a clinician at some point in their lives.The term eczema is broadly applied to a range of persistent skin conditions...
, and it is not uncommon for several or all of these diseases to affect one person. A number of studies suggest that vigorous eye rubbing contributes to the progression of keratoconus, and that patients should be discouraged from the practice. Iatrogenic
Iatrogenesis
Iatrogenesis, or an iatrogenic artifact is an inadvertent adverse effect or complication resulting from medical treatment or advice, including that of psychologists, therapists, pharmacists, nurses, physicians and dentists...
keratoconus has also been observed following LASIK
LASIK
LASIK or Lasik , commonly referred to simply as laser eye surgery, is a type of refractive surgery for correcting myopia, hyperopia, and astigmatism...
surgery, caused by removal of excessive stromal bed tissue.
Pathophysiology
Epithelium
Epithelium is one of the four basic types of animal tissue, along with connective tissue, muscle tissue and nervous tissue. Epithelial tissues line the cavities and surfaces of structures throughout the body, and also form many glands. Functions of epithelial cells include secretion, selective...
and stroma. As the two come into contact, cellular and structural changes in the cornea adversely affect its integrity and lead to the bulging and scarring that are characteristic of the disorder. Within any individual keratoconic cornea, there may be found regions of degenerative thinning coexisting with regions undergoing wound healing.
The visual distortion experienced by the patient comes from two sources, one being the irregular deformation of the surface of the cornea; the other being scarring that occurs on its exposed highpoints. These factors act to form regions on the cornea that map an image to different locations on the retina
Retina
The vertebrate retina is a light-sensitive tissue lining the inner surface of the eye. The optics of the eye create an image of the visual world on the retina, which serves much the same function as the film in a camera. Light striking the retina initiates a cascade of chemical and electrical...
and give rise to the symptom of monocular polyopia. The effect can worsen in low light conditions as the dark-adapted pupil
Pupil
The pupil is a hole located in the center of the iris of the eye that allows light to enter the retina. It appears black because most of the light entering the pupil is absorbed by the tissues inside the eye. In humans the pupil is round, but other species, such as some cats, have slit pupils. In...
dilates to expose more of the irregular surface of the cornea. Scarring appears to be an aspect of the corneal degradation; however, a recent, large, multi-center study suggests that abrasion by contact lenses may increase the likelihood of this finding by a factor of over two. A number of patients complain of chronic eye rubbing and also think it as a possible cause to the disease but it is not so; however, it has been observed that keratoconus progresses faster due to eye-rubbing.
A number of studies have indicated that keratoconic corneas show signs of increased activity by protease
Protease
A protease is any enzyme that conducts proteolysis, that is, begins protein catabolism by hydrolysis of the peptide bonds that link amino acids together in the polypeptide chain forming the protein....
s, a class of enzyme
Enzyme
Enzymes are proteins that catalyze chemical reactions. In enzymatic reactions, the molecules at the beginning of the process, called substrates, are converted into different molecules, called products. Almost all chemical reactions in a biological cell need enzymes in order to occur at rates...
s that break some of the collagen
Collagen
Collagen is a group of naturally occurring proteins found in animals, especially in the flesh and connective tissues of mammals. It is the main component of connective tissue, and is the most abundant protein in mammals, making up about 25% to 35% of the whole-body protein content...
cross-linkages in the stroma, with a simultaneous reduced expression
Gene expression
Gene expression is the process by which information from a gene is used in the synthesis of a functional gene product. These products are often proteins, but in non-protein coding genes such as ribosomal RNA , transfer RNA or small nuclear RNA genes, the product is a functional RNA...
of protease inhibitors
Enzyme inhibitor
An enzyme inhibitor is a molecule that binds to enzymes and decreases their activity. Since blocking an enzyme's activity can kill a pathogen or correct a metabolic imbalance, many drugs are enzyme inhibitors. They are also used as herbicides and pesticides...
. Other studies have suggested that reduced activity by the enzyme aldehyde dehydrogenase
Aldehyde dehydrogenase
Aldehyde dehydrogenases are a group of enzymes that catalyse the oxidation of aldehydes.- Function :Aldehyde dehydrogenase is a polymorphic enzyme responsible for the oxidation of aldehydes to carboxylic acids, which leave the liver and are metabolized by the body’s muscle and heart...
may be responsible for a build-up of free radicals and oxidising species in the cornea. It seems likely that, whatever the pathogenetical process
Pathogenesis
The pathogenesis of a disease is the mechanism by which the disease is caused. The term can also be used to describe the origin and development of the disease and whether it is acute, chronic or recurrent...
, the damage caused by activity within the cornea results in a reduction in its thickness and biomechanical strength. While keratoconus is considered a non-inflammatory disorder, one study shows that wearing rigid contact lenses by patients leads to overexpression of pro-inflammatory cytokine
Cytokine
Cytokines are small cell-signaling protein molecules that are secreted by the glial cells of the nervous system and by numerous cells of the immune system and are a category of signaling molecules used extensively in intercellular communication...
s, such as IL-6
Interleukin 6
Interleukin-6 is a protein that in humans is encoded by the IL6 gene.IL-6 is an interleukin that acts as both a pro-inflammatory and anti-inflammatory cytokine. It is secreted by T cells and macrophages to stimulate immune response, e.g. during infection and after trauma, especially burns or other...
, TNF-alpha, ICAM-1
ICAM-1
ICAM-1 also known as CD54 is a protein that in humans is encoded by the ICAM1 gene. This gene encodes a cell surface glycoprotein which is typically expressed on endothelial cells and cells of the immune system...
, and VCAM-1
VCAM-1
Vascular cell adhesion protein 1 also known as vascular cell adhesion molecule 1 or cluster of differentiation 106 is a protein that in humans is encoded by the VCAM1 gene...
in the tear fluid.
Contact lenses

Glasses
Glasses, also known as eyeglasses , spectacles or simply specs , are frames bearing lenses worn in front of the eyes. They are normally used for vision correction or eye protection. Safety glasses are a kind of eye protection against flying debris or against visible and near visible light or...
or soft contact lenses can suffice to correct for the mild astigmatism. As the condition progresses, these may no longer provide the patient with a satisfactory degree of visual acuity, and most clinical practitioners will move to managing the condition with rigid contact lenses, known as rigid gas-permeables
Rigid gas permeable
Rigid gas permeable lenses are rigid contact lenses made of oxygen-permeable polymers. Initially developed in the late 1970s, and through the 1980s and 1990s, they were an improvement over prior 'hard' lenses that restricted oxygen transmission to the eye....
, or RGPs. RGP lenses provide a good level of visual correction, but do not arrest progression of the condition.
In keratoconic patients, rigid contact lenses improve vision by means of tear fluid
Tears
Tears are secretions that clean and lubricate the eyes. Lacrimation or lachrymation is the production or shedding of tears....
filling the gap between the irregular corneal surface and the smooth regular inner surface of the lens, thereby creating the effect of a smoother cornea. Many specialized types of contact lenses have been developed for keratoconus, and affected people may seek out both doctors specialized in conditions of the cornea, and contact lens fitters who have experience managing patients with keratoconus. The irregular cone presents a challenge and the fitter will endeavour to produce a lens with the optimal contact, stability and steepness. Some trial-and-error fitting may prove necessary.
Traditionally, contact lenses for keratoconus have been the 'hard' or rigid gas-permeable variety, although manufacturers have also produced specialized 'soft' or hydrophilic lenses and, most recently, silicone hydrogel lenses. A soft lens has a tendency to conform to the conical shape of the cornea, thus diminishing its effect. To counter this, hybrid lenses have been developed which are hard in the centre and encompassed by a soft skirt. However, soft or earlier generation hybrid lenses did not prove effective for every patient. Early generation lenses like SoftPerm have been discontinued. The fourth generation of hybrid lens technology has improved significantly, giving more patients an option that combines the comfort of a soft lens with the visual acuity of an RGP lens. The new generation of technology fixes the issues that were prevalent in earlier generations and allows contact lenses to be fit for the majority of patients.
Some patients also find good vision correction and comfort with a "piggyback" lens combination, in which gas-permeable rigid lenses are worn over soft lenses, both providing a degree of vision correction. One form of piggyback lens makes use of a soft lens with a countersunk central area to accept the rigid lens. Fitting a piggyback lens combination requires experience on the part of the lens fitter, and tolerance on the part of the keratoconic patient.
Scleral lens
Scleral lens
A scleral lens is a large lens that rests on the Sclera and creates a Tear-filled vault over the Cornea. Scleral lenses are designed to treat a variety of eye conditions, many of which do not respond to other forms of treatment.- Design :...
es are sometimes prescribed for cases of advanced or very irregular keratoconus; these lenses cover a greater proportion of the surface of the eye and hence can offer improved stability. The larger size of the lenses may make them unappealing or uncomfortable to some; however, their easier handling can find favour with patients with reduced dexterity, such as the elderly.
Corneal transplant

Trephine
A trephine is a surgical instrument with a cylindrical blade. It can be of one of several dimensions and designs depending on what it is going to be used for. They may be specially designed for obtaining a cylindrically shaped core of bone that can be used for tests and bone studies, cutting holes...
s a lenticule of corneal tissue and then grafts
Medical grafting
Grafting refers to a surgical procedure to move tissue from one site to another on the body, or from another person, without bringing its own blood supply with it. Instead, a new blood supply grows in after it is placed. A similar technique where tissue is transferred with the blood supply intact...
the donor
Organ donation
Organ donation is the donation of biological tissue or an organ of the human body, from a living or dead person to a living recipient in need of a transplantation. Transplantable organs and tissues are removed in a surgical procedure following a determination, based on the donor's medical and...
cornea to the existing eye tissue, usually using a combination of running and individual sutures. The cornea does not have a direct blood supply, and so donor tissue is not required to be blood type
Blood type
A blood type is a classification of blood based on the presence or absence of inherited antigenic substances on the surface of red blood cells . These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system...
matched. Eye bank
Eye bank
Eye banks retrieve and store eyes for cornea transplants and research. US eye banks provide tissue for about 46,000 cornea transplants a year to treat conditions such as keratoconus and cornea scarring. The cornea is not the only part of the eye that can currently undergo transplantation. The...
s check the donor corneas for any disease or cellular irregularities.

In the USA, corneal transplants (also known as corneal grafts) for keratoconus are usually performed under sedation as outpatient surgery. In other countries, such as Australia and the UK, the operation is commonly performed with the patient undergoing a general anaesthetic. All cases require a careful follow-up with an eye surgeon (ophthalmologist) for a number of years. Frequently, vision is greatly improved after the surgery, but even if the actual visual acuity does not improve, because the cornea is a more normal shape after the healing is completed, patients can more easily be fitted with corrective lenses. Complications of corneal transplants are mostly related to vascularization of the corneal tissue and rejection
Transplant rejection
Transplant rejection occurs when transplanted tissue is rejected by the recipient's immune system, which destroys the transplanted tissue. Transplant rejection can be lessened by determining the molecular similitude between donor and recipient and by use of immunosuppressant drugs after...
of the donor cornea. Vision loss
Vision loss
Vision loss or visual loss is the absence of vision where it existed before, which can happen either acutely or chronically .-Ranges of vision loss:...
is very rare, though difficult-to-correct vision is possible. When rejection is severe, repeat transplants are often attempted, and are frequently successful. Keratoconus will not normally reoccur in the transplanted cornea; incidences of this have been observed, but are usually attributed to incomplete excision of the original cornea or inadequate screening of the donor tissue. The long-term outlook for corneal transplants performed for keratoconus is usually favorable once the initial healing period is completed and a few years have elapsed without problems.
Corneal ring segment inserts
A recent surgical alternative to corneal transplant is the insertion of intrastromal corneal ring segments. A small incision is made in the periphery of the cornea and two thin arcs of polymethyl methacrylate are slid between the layers of the stroma on either side of the pupilPupil
The pupil is a hole located in the center of the iris of the eye that allows light to enter the retina. It appears black because most of the light entering the pupil is absorbed by the tissues inside the eye. In humans the pupil is round, but other species, such as some cats, have slit pupils. In...
before the incision is closed. The segments push out against the curvature of the cornea, flattening the peak of the cone and returning it to a more natural shape. The procedure, carried out on an outpatient basis under local anaesthesia, offers the benefit of being reversible and even potentially exchangeable as it involves no removal of eye tissue.
The principal intrastromal ring available is known by the trade name of Intacs. Internationally, Ferrara Rings are also available. Intacs are a patented technology and are placed outside the optical zone versus the smaller prismatic Ferrara rings that are placed just inside the 5 mm optical zone. Intacs are the only corneal implants that have gone through the FDA Phase I, II and III clinical trials and were first approved by the Food and Drug Administration
Food and Drug Administration
The Food and Drug Administration is an agency of the United States Department of Health and Human Services, one of the United States federal executive departments...
(FDA) in the United States in 1999 for myopia
Myopia
Myopia , "shortsightedness" ) is a refractive defect of the eye in which collimated light produces image focus in front of the retina under conditions of accommodation. In simpler terms, myopia is a condition of the eye where the light that comes in does not directly focus on the retina but in...
; this was extended to the treatment of keratoconus in July 2004.

Infection
An infection is the colonization of a host organism by parasite species. Infecting parasites seek to use the host's resources to reproduce, often resulting in disease...
of the cornea, and migration or extrusion of the segments. The rings offer a good chance of vision improvement even in otherwise hard to manage eyes, but results are not guaranteed and in a few cases may worsen.
Early studies on intrastromal corneal rings involved use of two segments to cause global flattening of the cornea. A later study reported that better results could be obtained for those cones located more to the periphery of the cornea by using a single Intacs segment. This leads to preferential flattening of the cone below, but also to steepening the over-flat upper part of the cornea.
Corneal collagen crosslinking with riboflavin
A treatment developed at the Technische Universität Dresden, and which has shown early success is Corneal Collagen Crosslinking with Riboflavin, also known as CXL, CCR, CCL and KXL. A one-time application of riboflavinRiboflavin
Riboflavin, also known as vitamin B2 or additive E101, is an easily absorbed micronutrient with a key role in maintaining health in humans and animals. It is the central component of the cofactors FAD and FMN, and is therefore required by all flavoproteins. As such, vitamin B2 is required for a...
solution is administered to the eye and is activated by illumination with UV-A light for approximately 30 minutes. The riboflavin causes new bonds to form across adjacent collagen strands in the stromal layer of the cornea, which recovers and preserves some of the cornea's mechanical strength. The corneal epithelial layer is generally removed in order to increase penetration of the riboflavin into the stroma.
Clinical trial
Clinical trial
Clinical trials are a set of procedures in medical research and drug development that are conducted to allow safety and efficacy data to be collected for health interventions...
s are ongoing, but crosslinking is seeing increasing adoption by the ophthalmological community, and has shown success in retarding or stopping progression of the disease. Early results from an Australian study are very promising in reporting stabilization in all treated eyes, and a slight correction in visual acuity in most patients. The procedure, with epithelium removed, is approved for use throughout Europe, and commenced clinical trials in the USA in 2008. Over 300 patients have now been treated in the United States in those trials, which are composed of two randomized, controlled, multi-site clinical trials for the treatment of progressive keratoconus and post LASIK ectasia. Avedro Inc., the trial’s sponsor, is closing the follow-up phase of the study and completing the necessary steps to file the results with the FDA.
In some cases, collagen crosslinking may also be combined with other treatments to improve corneal asymmetry or optical refraction. Successful treatment methods include corneal ring segment inserts (INTACS or Ferrara Rings), Topography Guided Laser or Keraflex. Corrective lenses are normally required after these treatments but with smaller, more normalised prescriptions. Increased corneal symmetry allows for more comfortable contact lens wear, often of daily disposable lenses. These newer methods may have an important role in limiting deterioration of vision, increasing unaided/uncorrected vision and reducing the case for corneal transplantation.
Radial keratotomy
Radial keratotomy is a refractive surgeryRefractive surgery
Refractive eye surgery is any eye surgery used to improve the refractive state of the eye and decrease or eliminate dependency on glasses or contact lenses. This can include various methods of surgical remodeling of the cornea or cataract surgery. The most common methods today use excimer lasers to...
procedure where the surgeon makes a spoke-like pattern of incisions into the cornea to modify its shape. This early surgical option for myopia
Myopia
Myopia , "shortsightedness" ) is a refractive defect of the eye in which collimated light produces image focus in front of the retina under conditions of accommodation. In simpler terms, myopia is a condition of the eye where the light that comes in does not directly focus on the retina but in...
has been largely superseded by LASIK
LASIK
LASIK or Lasik , commonly referred to simply as laser eye surgery, is a type of refractive surgery for correcting myopia, hyperopia, and astigmatism...
and other similar procedures. LASIK itself is absolutely contraindicated in keratoconus and other corneal thinning conditions as removal of corneal stromal tissue will further damage an already thin and weak cornea.
For similar reasons, radial keratotomy has also generally not been used for keratoconic patients. However, an Italian clinic has reported some success with a modified asymmetric radial keratotomy procedure, in which the incisions are confined to one sector of the eye. The corneal thickness is first measured using a pachymeter
Pachymeter
A pachymeter is a medical device used to measure the thickness of the eye's cornea. It is used to perform Corneal pachymetry prior to LASIK surgery, for Keratoconus screening, LRI surgery and is useful in screening for patients suspected of developing glaucoma among other uses.Modern devices use...
, then the surgeon makes cuts to a depth of 70–80% of the measured thickness. The patient may initially experience photophobia
Photophobia
Photophobia is a symptom of abnormal intolerance to visual perception of light. As a medical symptom photophobia is not a morbid fear or phobia, but an experience of discomfort or pain to the eyes due to light exposure or by presence of actual physical photosensitivity of the eyes, though the term...
and fluctuation of vision, in common with other forms of refractive surgery. This technique has yet to go through the official experimentation and follow-up period which is generally required by the Italian National Health Service to accept a new surgery technique before it can be offered to patients.
DALK transplants
One way of reducing the risk of rejection is to use a newer technique called a Deep Anterior Lamellar Keratoplasty, referred to as DALK. In a DALK graft, only the outermost epithelium and the main bulk of the cornea, the stroma, are replaced; the patient's rearmost endotheliumCorneal endothelium
The corneal endothelium is a single layer of cells on the inner surface of the cornea. It faces the chamber formed between the cornea and the iris....
layer and the Descemet's membrane are left, giving some additional structural integrity to the post-graft cornea. Furthermore, it is possible to transplant tissue from a donor which has been freeze-dried
Freeze drying
Freeze-drying is a dehydration process typically used to preserve a perishable material or make the material more convenient for transport...
. The freeze-drying process ensures that this tissue is dead, so there is no chance of a rejection.
Some surgeons prefer to remove the donor epithelium, others leave the donor's cells in place. Removing it can cause a slight improvement in overall vision, but a corresponding increase in visual recovery time.
Epikeratophakia
Rarely, a non-penetrating keratoplasty known as an epikeratophakia (or epikeratoplasty) may be performed in cases of keratoconus. The corneal epithelium is removed and a lenticule of donor cornea grafted on top of it. The procedure requires a greater level of skill on the part of the surgeon, and is less frequently performed than a penetrating keratoplasty as the outcome is generally less favorable. However, it may be seen as an option in a number of cases, particularly for young patients.Prognosis
Astigmatism (eye)
Astigmatism is an optical defect in which vision is blurred due to the inability of the optics of the eye to focus a point object into a sharp focused image on the retina. This may be due to an irregular or toric curvature of the cornea or lens. There are two types of astigmatism: regular and...
and myopia, commonly at the onset of puberty
Puberty
Puberty is the process of physical changes by which a child's body matures into an adult body capable of reproduction, as initiated by hormonal signals from the brain to the gonads; the ovaries in a girl, the testes in a boy...
, and are diagnosed by the late teenage years or early 20s. The disease can however present or progress at any age: in rare cases keratoconus can present in children or not until later adulthood. A diagnosis of the disease at an early age may indicate a greater risk of severity in later life. Patients' vision will seem to fluctuate over a period of months, driving them to change lens prescriptions frequently, but as the condition worsens, contact lens
Contact lens
A contact lens, or simply contact, is a lens placed on the eye. They are considered medical devices and can be worn to correct vision, for cosmetic or therapeutic reasons. In 2004, it was estimated that 125 million people use contact lenses worldwide, including 28 to 38 million in the United...
es are required in the majority of cases. The course of the disorder can be quite variable, with some patients remaining stable for years or indefinitely, while others progress rapidly or experience occasional exacerbations over a long and otherwise steady course. It tends to progress more rapidly in patients when the first presentation is in second decade of life. Most commonly, keratoconus progresses for a period of ten to twenty years before the course of the disease generally ceases in the third and fourth decades of life.
_due_to_keratoconus.jpg)
Descemet's membrane
Descemet's membrane is the basement membrane that lies between the corneal proper substance, also called stroma, and the endothelial layer of the cornea. It is composed of a different kind of collagen than the stroma. The endothelial layer is located at the posterior of the cornea...
, an inner layer of the cornea. Aqueous humor from the eye's anterior chamber
Anterior chamber
The anterior chamber is the fluid-filled space inside the eye between the iris and the cornea's innermost surface, the endothelium. Aqueous humor is the fluid that fills the anterior chamber. Hyphema and glaucoma are two main pathologies in this area. In hyphema, blood fills the anterior chamber...
seeps into the cornea before Descemet's membrane reseals. The patient experiences pain and a sudden severe clouding of vision, with the cornea taking on a translucent milky-white appearance known as a corneal hydrops. Although disconcerting to the patient, the effect is normally temporary and after a period of six to eight weeks the cornea usually returns to its former transparency. The recovery can be aided non-surgically by bandaging with an osmotic
Osmosis
Osmosis is the movement of solvent molecules through a selectively permeable membrane into a region of higher solute concentration, aiming to equalize the solute concentrations on the two sides...
saline
Saline (medicine)
In medicine, saline is a general term referring to a sterile solution of sodium chloride in water but is only sterile when it is to be placed intravenously, otherwise, a saline solution is a salt water solution...
solution. Although a hydrops usually causes increased scarring of the cornea, occasionally it will benefit a patient by creating a flatter cone, aiding the fitting of contact lenses. Occasionally, the cornea thins to the point that a partial rupture occurs at the level of Descemet´s membrane, resulting in a small, bead-like swelling on the cornea that may become filled with fluid (cornea hydropsy). When this occurs, severe vision decrease may occur until the edema slowly resolves. Corneal transplantation is not usually indicated while the hydropsy persists.
Epidemiology
The National Eye InstituteNational Eye Institute
The National Eye Institute is one of the US National Institutes of Health that was established in 1968. The mission of NEI is to prolong and protect the vision of the American people. The NEI conducts and performs research into treating and preventing diseases affecting the eye or vision....
reports that keratoconus is the most common corneal dystrophy
Corneal dystrophy
Corneal dystrophy is a group of disorders, characterised by a noninflammatory, inherited, bilateral opacity of the transparent front part of the eye called the cornea.The distrophies could be subdivided based on specie affected:...
in the United States, affecting approximately 1 in 2,000 Americans, but some reports place the figure as high as 1 in 500. The inconsistency may be due to variations in diagnostic criteria, with some cases of severe astigmatism interpreted as those of keratoconus, and vice versa. A long-term study found a mean incidence rate of 2.0 new cases per 100,000 population per year. It is suggested that males and females, and all ethnicities appear equally susceptible, though some recent studies have cast doubt upon this, suggesting a higher prevalence amongst females; the literature, however, varying as to its extent. Also, a study carried out in the UK suggests that people of a South Asian heritage are 4.4 times as likely to suffer from keratoconus as Caucasians, and are also more likely to be affected with the condition earlier.
Keratoconus is normally bilateral (affecting both eyes) although the distortion is usually asymmetric and is rarely completely identical in both corneas. Unilateral cases tend to be uncommon, and may in fact be very rare if a very mild condition in the better eye is simply below the limit of clinical detection. It is common for keratoconus to be diagnosed first in one eye and not until later in the other. As the condition then progresses in both eyes, the vision in the earlier-diagnosed eye will often persist to be poorer than that in its fellow.
History
Ophthalmology
Ophthalmology is the branch of medicine that deals with the anatomy, physiology and diseases of the eye. An ophthalmologist is a specialist in medical and surgical eye problems...
Burchard Mauchart
Burchard Mauchart
Burchard David Mauchart was professor of anatomy and surgery at the University of Tübingen, Germany, and a pioneer in the field of ophthalmology. In 1748 he became one of the first to document the eye disorder now known as keratoconus. His surviving works are now to be found in the form of theses...
provided an early description of a case of keratoconus, which he called staphyloma diaphanum. However, it was not until 1854 that British physician John Nottingham clearly described keratoconus and distinguished it from other ectasia
Ectasia
Dilation or distention of a tubular structure. It occurs as part of a pathophysiological process.-Specific conditions:* Duct ectasia of breast, a dilated milk duct...
s of the cornea. Nottingham reported the cases of "conical cornea" that had come to his attention, and described several classic features of the disease, including polyopia
Diplopia
Diplopia, commonly known as double vision, is the simultaneous perception of two images of a single object that may be displaced horizontally, vertically, or diagonally in relation to each other...
, weakness of the cornea, and difficulty matching corrective lenses to the patient's vision. In 1859 British surgeon William Bowman used an ophthalmoscope (recently invented by Hermann von Helmholtz
Hermann von Helmholtz
Hermann Ludwig Ferdinand von Helmholtz was a German physician and physicist who made significant contributions to several widely varied areas of modern science...
) to diagnose keratoconus, and described how to angle the instrument's mirror so as to best see the conical shape of the cornea. Bowman also attempted to restore the vision by pulling on the iris
Iris (anatomy)
The iris is a thin, circular structure in the eye, responsible for controlling the diameter and size of the pupils and thus the amount of light reaching the retina. "Eye color" is the color of the iris, which can be green, blue, or brown. In some cases it can be hazel , grey, violet, or even pink...
with a fine hook inserted through the cornea and stretching the pupil
Pupil
The pupil is a hole located in the center of the iris of the eye that allows light to enter the retina. It appears black because most of the light entering the pupil is absorbed by the tissues inside the eye. In humans the pupil is round, but other species, such as some cats, have slit pupils. In...
into a vertical slit, like that of a cat. He reported that he had had a measure of success with the technique, restoring vision to an 18-year old woman who had previously been unable to count fingers at a distance of 8 inches (20 cm). By 1869, when the pioneering Swiss ophthalmologist Johann Horner wrote a thesis entitled On the treatment of keratoconus, the disorder had acquired its current name. The treatment at that time, endorsed by the leading German ophthalmologist Albrecht von Graefe, was an attempt to physically reshape the cornea by chemical cauterization with a silver nitrate
Silver nitrate
Silver nitrate is an inorganic compound with chemical formula . This compound is a versatile precursor to many other silver compounds, such as those used in photography. It is far less sensitive to light than the halides...
solution and application of a miosis
Miosis
Miosis is the constriction of the pupil of the eye to two millimeters or less...
-causing agent with a pressure dressing. In 1888 the treatment of keratoconus became one of the first practical applications of the then newly invented contact lens
Contact lens
A contact lens, or simply contact, is a lens placed on the eye. They are considered medical devices and can be worn to correct vision, for cosmetic or therapeutic reasons. In 2004, it was estimated that 125 million people use contact lenses worldwide, including 28 to 38 million in the United...
, when the French physician Eugène Kalt
Eugène Kalt
Eugène Kalt was a French ophthalmologist who developed the first known application of a contact lens for the correction of keratoconus. In 1888, he worked on a crude flat-fitting glass scleral lenses designed to "compress the steep conical apex thereby correcting the condition"...
manufactured a glass scleral shell which improved vision by compressing the cornea into a more regular shape. Since the start of the twentieth century, research on keratoconus has both improved understanding of the disease and greatly expanded the range of treatment options. The first successful transplantation of cornea to treat keratoconus was done in 1936 by Ramon Castroviejo
Ramon Castroviejo
Ramón Castroviejo Briones was a famous Spanish and American eye surgeon remembered for his achievements in corneal transplantation.-Biography:Born in Logroño, Spain he received his medical education at the University of Madrid...
.
Related disorders
Several other non-inflammatory eye disorders, generally rarer than keratoconus, also cause thinning of the cornea:Keratoglobus
Keratoglobus
Keratoglobus , is a degenerative non-inflammatory disorder of the eye in which structural changes within the cornea cause it to become extremely thin and change to a more globular shape than its normal gradual curve...
- Keratoglobus is a very rare condition that causes corneal thinning primarily at the margins, resulting in a spherical, slightly enlarged eye. It may be genetically related to keratoconus.
Pellucid Marginal Degeneration
Pellucid Marginal Degeneration
Pellucid Marginal Degeneration , is a degenerative corneal condition, often confused with keratoconus. It is typically characterized by a bilateral thinning in the periphery of the cornea, that is non-inflammatory, although unilateral cases have been reported...
- Pellucid marginal degeneration causes thinning of a narrow (1–2 mm) band of the cornea, usually along the inferior corneal margin. It causes irregular astigmatism that can often be corrected by spectacles. Differential diagnosis may be made by slit-lamp examination.
Posterior keratoconus
- Keratoconus and posterior keratoconus are distinct disorders, despite their similar names. Posterior keratoconus is a rare abnormality, usually congenital, which causes a non-progressive thinning of the inner surface of the cornea, while the curvature of the anterior surface remains normal. Normally only a single eye is affected.
See also
- List of eye diseases and disorders
- OphthalmologyOphthalmologyOphthalmology is the branch of medicine that deals with the anatomy, physiology and diseases of the eye. An ophthalmologist is a specialist in medical and surgical eye problems...
External links
- Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study
- Facts About the Cornea and Corneal Disease The National Eye Institute (NEI)
- KCVision What people with keratoconus see (images)
- Keratoconus Experience - Views of a Patients Eye
- The Global Keratoconus Foundation
- Keratoconus Australia
- National Keratoconus Foundation (US)
- Information from Keratoconus Self Help and Support Group (UK)
- Experiences Symptoms and Progressions from patients view (PeerMade.info IN)
- Nederlandstalige Lotgenoten Keratoconus (NL)
- Keratoconus and Corneal Transplantation - An Educated Patient's Journey (US)

