
Tracheobronchial injury
Encyclopedia
Tracheobronchial injury (TBI) is damage to the tracheobronchial tree
(the airway
structure involving the trachea
and bronchi
). It can result from blunt
or penetrating
trauma to the neck or chest
, inhalation of harmful fumes or smoke
, or aspiration
of liquids or objects.
Though rare, TBI is a serious condition; it may cause obstruction of the airway with resulting life-threatening respiratory insufficiency
. Other injuries accompany TBI in about half of cases. Of those people with TBI who die, most do so before receiving emergency care, either from airway obstruction, exsanguination
, or from injuries to other vital organs. Of those who do reach a hospital, the mortality rate
may be as high as 30%.
TBI is frequently difficult to diagnose
and treat. Early diagnosis is important to prevent complications
, which include stenosis
(narrowing) of the airway, respiratory tract infection
, and damage to the lung tissue. Diagnosis involves procedures such as bronchoscopy
, radiography
, and x-ray computed tomography to visualize the tracheobronchial tree. Signs
and symptom
s vary based on the location and severity of the injury; they commonly include dyspnea
(difficulty breathing), dysphonia
(a condition where the voice can be hoarse, weak, or excessively breathy), coughing, and abnormal breath sounds. In the emergency setting, tracheal intubation
can be used to ensure that the airway remains open. In severe cases, surgery may be necessary to repair a TBI.
and the center of the chest, where it splits into the two bronchi at a ridge called the carina
. The trachea is stabilized and kept open by rings made of cartilage
that surround the front and sides of the structure; these rings are not closed and do not surround the back, which is made of membrane. The bronchi split into smaller branches and then to bronchioles that supply air to the alveoli
, the tiny air-filled sacs in the lungs responsible for absorbing oxygen
. An arbitrary division can be made between the intrathoracic
and cervical
trachea at the thoracic inlet
, an opening at the top of the thoracic cavity
. Anatomical structures that surround and protect the tracheobronchial tree include the lungs, the esophagus
, large blood vessels, the rib cage
, the thoracic spine
, and the sternum. Children have softer tracheas and a more elastic tracheobronchial trees than adults; this elasticity, which helps protect the structures from injury when they are compressed, may contribute to the lower incidence
of TBI in children.
, occurring between the rings of the trachea, longitudinal or spiral. They may occur along the membranous part of the trachea, the main bronchi, or both. In 8% of ruptures, lesions are complex, occurring in more than one location, with more than one type of lesion, or on both of the main bronchi and the trachea. Transverse tears are more common than longitudinal or complex ones. The laceration may completely transect the airway or it may go only partway around. Partial tears that do not go all the way around the circumference of the airway do not allow a lacerated airway to become completely detached; tears that encircle the whole airway can allow separation to occur. Lacerations may also be classified as complete or incomplete. In an incomplete lesion, a layer of tissue surrounding the bronchus remains intact and can keep the air in the airway, preventing it from leaking into the areas surrounding the airways. Incomplete lacerations may require closer scrutiny to detect and may not be diagnosed right away.
Bronchial injuries are divided into those that are accompanied by a disruption of the pleura
and those that are not; in the former, air can leak from the hole in the airway and a pneumothorax
can form. The latter type is associated with more minor signs; pneumothorax is small if it occurs at all, and although function is lost in the part of the lung supplied by the injured bronchus, unaffected parts of the lungs may be able to compensate.
Most TBI that results from blunt trauma occurs within the chest. The most common tracheal injury is a tear near the carina or in the membranous wall of the trachea. In blunt chest trauma, TBI occurs within 2.5 cm of the carina 40–80% of the time. The injury is more common in the right main bronchus than the left, possibly because the former is near vertebrae
, which may injure it. Also, the aorta
and other tissues in the mid chest that surround the left main bronchus may protect it. Another possibility is that people with left main bronchus injuries are more likely to also have other deadly injuries and therefore die before reaching hospital, making them less likely to be included in studies that determine rates of injuries.
 Signs and symptoms vary depending on what part of the tracheobronchial tree is injured and how severely it is damaged. There are no direct signs of TBI, but certain signs suggest the injury and raise a clinician's suspicion that it has occurred. Many of the signs and symptoms are also present in injuries with similar injury mechanisms such as pneumothorax. Dyspnea and respiratory distress are found in 76–100% of people with TBI, and coughing up blood
Signs and symptoms vary depending on what part of the tracheobronchial tree is injured and how severely it is damaged. There are no direct signs of TBI, but certain signs suggest the injury and raise a clinician's suspicion that it has occurred. Many of the signs and symptoms are also present in injuries with similar injury mechanisms such as pneumothorax. Dyspnea and respiratory distress are found in 76–100% of people with TBI, and coughing up blood
has been found in up to 25%. However, isolated TBI does not usually cause profuse bleeding; if such bleeding is observed it is likely to be due to another injury such as a ruptured large blood vessel
. The patient may exhibit dysphonia or have diminished breath sounds, and rapid breathing
is common. Coughing may be present, and stridor
, an abnormal, high-pitched breath sound indicating obstruction of the upper airway can also occur.
Damage to the airways can cause subcutaneous emphysema
(air trapped in the subcutaneous tissue
of the skin) in the abdomen, chest, neck, and head. Subcutaneous emphysema, present in up to 85% of people with TBI, is particularly indicative of the injury when it is only in the neck. Air is trapped in the chest cavity outside the lungs (pneumothorax) in about 70% of TBI. Especially strong evidence that TBI has occurred is failure of a pneumothorax to resolve even when a chest tube
is placed to rid the chest cavity of the air; it shows that air is continually leaking into the chest cavity from the site of the tear. Air can also be trapped in the mediastinum
, the center of the chest cavity (pneumomediastinum
). If air escapes from a penetrating injury to the neck, a definite diagnosis of TBI can be made. Hamman's sign
, a sound of crackling that occurs in time with the heartbeat, may also accompany TBI.
, but are more often the result of blunt trauma. TBI due blunt forces usually results from high-energy impacts such as falls from height and motor vehicle accidents; the injury is rare in low-impact mechanisms. Injuries of the trachea cause about 1% of traffic-related deaths. Other potential causes are falls from high places and injuries in which the chest is crushed. Explosions are another cause.
Gunshot wounds are the commonest form of penetrating trauma that cause TBI. Less commonly, knife wounds and shrapnel from motor vehicle accidents can also penetrate the airways. Most injuries to the trachea occur in the neck, because the airways within the chest are deep and therefore well protected; however, up to a quarter of TBI resulting from penetrating trauma occurs within the chest. Injury to the cervical trachea usually affects the anterior (front) part of the trachea.
Certain medical procedures can also injure the airways; these include tracheal intubation, bronchoscopy, and tracheotomy
. The back of the trachea may be damaged during tracheotomy. TBI resulting from tracheal intubation (insertion of a tube into the trachea) is rare, and the mechanism by which it occurs is unclear. However, one likely mechanism involves an endotracheal tube
catching in a fold of membrane and tearing it as it is advanced downward through the airway. When an endotracheal tube tears the trachea, it typically does so at the posterior (back) membranous wall. Unlike TBI that results from blunt trauma, most iatrogenic injuries to the airway involve longitudinal tears to the back of the trachea or tears on the side that pull the membranous part of the trachea away from the cartilage. Excessive pressure from the cuff of an endotracheal tube can reduce blood supply to the tissues of the trachea, leading to ischemia
and potentially causing it to become ulcerated, infected
, and, later, narrowed.
The mucosal lining
of the trachea may also be injured by inhalation of hot gases or harmful fumes such as chlorine gas
. This can lead to edema
(swelling), necrosis
(death of the tissue), scar formation, and ultimately stenosis. However, TBI due to inhalation, foreign body aspiration, and medical procedures is uncommon.
of the neck, usually resulting from vehicle crashes, can also injure the trachea, and trauma to the neck can crush the trachea against the vertebrae. A crush injury of the larynx or cervical trachea can occur in head-on collisions when the neck is hyperextended and strikes the steering wheel or dashboard; this has been called a "dashboard injury". The larynx and cervical trachea may also be injured in front-on collisions by the seat belt.
Although the mechanism is not well understood, TBI due to blunt trauma is widely thought to be caused by any combination of three possible mechanisms: an increase in pressure within the airways, shearing
, and pulling apart. The first type of injury, sometimes called an "explosive rupture", may occur when the chest is violently compressed, for example when a driver strikes the steering wheel in a vehicle accident or when the chest is crushed. The pressure in the airways, especially the larger airways (the trachea and bronchi), quickly rises as a result of the compression, because the glottis
reflexively closes off the airways. When this pressure exceeds the elasticity of the tissues, they burst; thus the membranous part of the trachea is more commonly affected by this mechanism of injury than cartilaginous portions.
The second mechanism may occur when the chest is suddenly decelerated
, as occurs in vehicle accidents, producing a shearing force. The lungs are mobile in the chest cavity but their movement is more restricted near the hilum
. Areas near the cricoid cartilage and carina are fixed to the thyroid cartilage
and the pericardium
respectively; thus if the airways move, they can tear at these points of fixation.
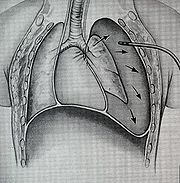
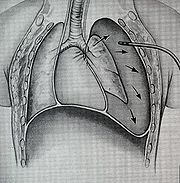
The third mechanism occurs when the chest is compressed from front to back, causing it to widen from side to side. The lungs adhere to the chest wall because of the negative pressure between them and the pleural membranes lining the inside of the chest cavity; thus when the chest widens, they are pulled apart. This creates tension at the carina; the airway tears if this tensile force exceeds its elasticity. This mechanism may be the cause of injury when the chest is crushed. Most TBI are probably due to a combination of these three mechanisms.
When airways are damaged, air can escape from them and be trapped in the surrounding tissues in the neck (subcutaneous emphysema) and mediastinum (pneumomediastinum); if it builds up to high enough pressures there, it can compress the airways. Massive air leaks from a ruptured airway can also compromise the circulation by preventing blood from returning to the heart from the head and lower body; this causes a potentially deadly reduction in the amount of blood the heart is able to pump out. Blood and other fluids can build up in the airways, and the injury can interfere with the patency of the airway and interfere with its continuity. However, even if the trachea is completely transected, the tissues surrounding it may hold it together enough for adequate air exchange to occur, at least at first.
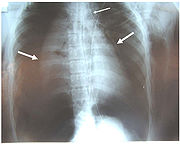
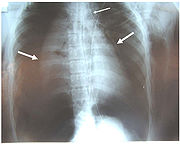
Chest x-ray is the initial imaging technique used to diagnose TBI. The film may not have any signs in an otherwise asymptomatic patient. Indications of TBI seen on radiographs include deformity in the trachea or a defect in the tracheal wall. Radiography may also show cervical emphysema, air in the tissues of the neck. X-rays may also show accompanying injuries and signs such as fractures and subcutaneous emphysema. If subcutaneous emphysema occurs and the hyoid bone
appears in an X-ray to be sitting unusually high in the throat, it may be an indication that the trachea has been severed. TBI is also suspected if an endotracheal tube appears in an X-ray to be out of place, or if its cuff appears to be more full than normal or to protrude through a tear in the airway. If a bronchus is torn all the way around, the lung may collapse outward toward the chest wall (rather than inward, as it usually does in pneumothorax) because it loses the attachment to the bronchus which normally holds it toward the center. In a person lying face-up, the lung collapses toward the diaphragm
and the back. This sign, described in 1969, is called fallen lung sign and is pathognomonic
of TBI (that is, it is diagnostic for TBI because it does not occur in other conditions); however it occurs only rarely. In as many as one in five cases, people with blunt trauma and TBI have no signs of the injury on chest X-ray. CT scanning detects over 90% of TBI resulting from blunt trauma, but neither X-ray nor CT are a replacement for bronchoscopy.
At least 30% of TBI are not discovered at first; this number may be as high as 50%. In about 10% of cases, TBI has no specific signs either clinically or on chest radiography, and its detection may be further complicated by concurrent injuries, since TBI tends to occur after high-energy accidents. Weeks or months may go by before the injury is diagnosed, even though the injury is better known than it was in the past.
 Treatment of TBI varies based on the location and severity of injury and whether the patient is stable or having trouble breathing, but ensuring that the airway is patent so that the patient can breathe is always of paramount importance. Ensuring an open airway and adequate ventilation may be difficult in people with TBI. Intubation, one method to secure the airway, may be used to bypass a disruption in the airway in order to send air to the lungs. If necessary, a tube can be placed into the uninjured bronchus, and a single lung can be ventilated. If there is a penetrating injury to the neck through which air is escaping, the trachea may be intubated through the wound. Multiple unsuccessful attempts at conventional (direct) laryngoscopy
Treatment of TBI varies based on the location and severity of injury and whether the patient is stable or having trouble breathing, but ensuring that the airway is patent so that the patient can breathe is always of paramount importance. Ensuring an open airway and adequate ventilation may be difficult in people with TBI. Intubation, one method to secure the airway, may be used to bypass a disruption in the airway in order to send air to the lungs. If necessary, a tube can be placed into the uninjured bronchus, and a single lung can be ventilated. If there is a penetrating injury to the neck through which air is escaping, the trachea may be intubated through the wound. Multiple unsuccessful attempts at conventional (direct) laryngoscopy
may threaten the airway, so alternative techniques to visualize the airway, such as fiberoptic or video laryngoscopy, may be employed to facilitate tracheal intubation. If the upper trachea is injured, an incision can be made in the trachea (tracheotomy) or the cricothyroid membrane
(cricothyrotomy
, or cricothyroidotomy) in order to ensure an open airway. However, cricothyrotomy may not be useful if the trachea is lacerated below the site of the artificial airway. Tracheotomy is used sparingly because it can cause complications such as infections and narrowing of the trachea and larynx. When it is impossible to establish a sufficient airway, or when complicated surgery must be performed, cardiopulmonary bypass may be used—blood is pumped out of the body, oxygenated
by a machine, and pumped back in. If a pneumothorax occurs, a chest tube may be inserted into the pleural cavity to remove the air.
 People with TBI are provided with supplemental oxygen and may need mechanical ventilation
People with TBI are provided with supplemental oxygen and may need mechanical ventilation
. Employment of certain measures such as Positive end-expiratory pressure
(PEEP) and ventilation at higher-than-normal pressures may be helpful in maintaining adequate oxygenation. However, such measures can also increase leakage of air through a tear, and can stress the sutures in a tear that has been surgically repaired; therefore the lowest possible airway pressures that still maintain oxygenation are typically used. Mechanical ventilation can also cause pulmonary barotrauma when high pressure is required to ventilate the lungs. Techniques such as pulmonary toilet
(removal of secretion
s), fluid management, and treatment of pneumonia are employed to improve pulmonary compliance
(the elasticity of the lungs).
While TBI may be managed without surgery, surgical repair of the tear is considered standard in the treatment of most TBI. It is required if a tear interferes with ventilation; if mediastinitis
(inflammation of the tissues in the mid-chest) occurs; or if subcutaneous or mediastinal emphysema progresses rapidly; or if air leak or large pneumothorax is persistent despite chest tube placement. Other indications for surgery are a tear more than one third the circumference of the airway, tears with loss of tissue, and a need for positive pressure ventilation. Damaged tissue around a rupture (e.g. torn or scarred tissue) may be removed in order to obtain clean edges that can be surgically repaired. Debridement
of damaged tissue can shorten the trachea by as much as 50%. Repair of extensive tears can include sewing a flap of tissue taken from the membranes surrounding the heart or lungs (the pericardium and pleura, respectively) over the sutures to protect them. When lung tissue is destroyed as a result of TBI complications, pneumonectomy
or lobectomy
(removal of a lung or of one lobe, respectively) may be required. Pneumonectomy is avoided whenever possible due to the high rate of death associated with the procedure. Surgery to repair a tear in the tracheobronchial tree can be successful even when it is performed months after the trauma, as can occur if the diagnosis of TBI is delayed. When airway stenosis results after delayed diagnosis, surgery is similar to that performed after early diagnosis: the stenotic section is removed and the cut airway is repaired.
 Most people with TBI who die do so within minutes of the injury, due to complications such as pneumothorax and insufficient airway and to other injuries that occurred at the same time. Most late deaths that occur in TBI are attributed to sepsis
Most people with TBI who die do so within minutes of the injury, due to complications such as pneumothorax and insufficient airway and to other injuries that occurred at the same time. Most late deaths that occur in TBI are attributed to sepsis
or multiple organ dysfunction syndrome
(MODS). If the condition is not recognized and treated early, serious complications are more likely to occur; for example, pneumonia
and bronchiectasis
may occur as late complications. Years can pass before the condition is recognized. Some TBI are so small that they do not have significant clinical manifestations; they may never be noticed or diagnosed and may heal without intervention.
If granulation tissue
grows over the injured site, it can cause stenosis of the airway, after a week to a month. The granulation tissue must be surgically excised. Delayed diagnosis of a bronchial rupture increases risk of infection and lengthens hospital stay. People with a narrowed airway may suffer dyspnea, coughing, wheezing
, respiratory tract infection, and difficulty with clearing secretions. If the bronchiole is completely obstructed, atelectasis
occurs: the alveoli of the lung collapse. Lung tissue distal to a completely obstructed bronchiole often does not become infected. Because it is filled with mucus, this tissue remains functional. When the secretions are removed, the affected portion of the lung is commonly able to function almost normally. However, infection is common in lungs distal to a partially obstructed bronchiole. Infected lung tissue distal to a stricture can be damaged, and wheezing and coughing may develop due to the narrowing. In addition to pneumonia, the stenosis may cause bronchiectasis, in which bronchi are dilated, to develop. Even after an airway with a stricture is restored to normal, the resulting loss of lung function may be permanent.
Complications may also occur with treatment; for example a granuloma
can form at the suture site. Also, the sutured wound can tear again, as occurs when there is excessive pressure in the airways from ventilation. However, for people who do receive surgery soon after the injury to repair the lesion, outcome is usually good; the long-term outcome is good for over 90% of people who have TBI surgically repaired early in treatment. Even when surgery is performed years after the injury, the outlook is good, with low rates of death and disability and good chances of preserving lung function.
s have TBI. The incidence is estimated at 2% in blunt chest and neck trauma and 1–2% in penetrating chest trauma. Laryngotracheal injuries occur in 8% of patients with penetrating injury to the neck, and TBI occurs in 2.8% of blunt chest trauma deaths. In people with blunt trauma who do reach a hospital alive, reports have found incidences of 2.1% and 5.3%. Another study of blunt chest trauma revealed an incidence of only 0.3%, but a mortality rate of 67% (possibly due in part to associated injuries). The incidence of iatrogenic TBI (that caused by medical procedures) is rising, and the risk may be higher for women and the elderly. TBI results about once every 20,000 times someone is intubated through the mouth, but when intubation is performed emergently, the incidence may be as high as 15%.
The mortality rate for people who reach a hospital alive was estimated at 30% in 1966; more recent estimates place this number at 9%. The number of people reaching a hospital alive has increased, perhaps due to improved prehospital
care or specialized treatment centers. Of those who reach the hospital alive but then die, most do so within the first two hours of arrival. The sooner a TBI is diagnosed, the higher the mortality rate; this is likely due to other accompanying injuries that prove fatal.
Accompanying injuries often play a key role in the outcome. Injuries that may accompany TBI include pulmonary contusion
and laceration
; and fractures of the sternum
, ribs
and clavicles
. Spinal cord injury
, facial trauma
, traumatic aortic rupture
, injuries to the abdomen
, lung, and head
are present in 40–100%. The most common accompanying injury is esophageal perforation or rupture (known as Boerhaave syndrome
), which occurs in as many as 43% of the penetrating injuries to the neck that cause tracheal injury.
of the right bronchus. Long-term survival of the injury was unknown in humans until a report was made of a person who survived in 1927. In 1931, a report made by Nissen described successful removal of a lung in a 12-year-old girl who had had narrowing of the bronchus due to the injury. Repair of TBI was probably first attempted in 1945, when the first documented case of a successful suturing of a lacerated bronchus was made. Prior to 1950, the mortality rate was 36%; it had fallen to 9% by 2001; this improvement was likely due to improvements in treatments and surgical techniques, including those for injuries commonly associated with TBI.
Tracheobronchial tree
The tracheobronchial tree is the structure from the trachea, bronchi, and bronchioles that forms the airways that supply air to the lungs. It is within the neck and the chest. The structure looks like a tree because the trachea splits into the right and left mainstem bronchi, which "branch" into...
(the airway
Airway
The pulmonary airway comprises those parts of the respiratory system through which air flows, conceptually beginning at the nose and mouth, and terminating in the alveoli...
structure involving the trachea
Vertebrate trachea
In tetrapod anatomy the trachea, or windpipe, is a tube that connects the pharynx or larynx to the lungs, allowing the passage of air. It is lined with pseudostratified ciliated columnar epithelium cells with goblet cells that produce mucus...
and bronchi
Bronchus
A bronchus is a passage of airway in the respiratory tract that conducts air into the lungs. The bronchus branches into smaller tubes, which in turn become bronchioles....
). It can result from blunt
Blunt trauma
In medical terminology, blunt trauma, blunt injury, non-penetrating trauma or blunt force trauma refers to a type of physical trauma caused to a body part, either by impact, injury or physical attack; the latter usually being referred to as blunt force trauma...
or penetrating
Penetrating trauma
Penetrating trauma is an injury that occurs when an object pierces the skin and enters a tissue of the body, creating an open wound. In blunt, or non-penetrating trauma, there may be an impact, but the skin is not necessarily broken. The penetrating object may remain in the tissues, come back out...
trauma to the neck or chest
Chest trauma
Chest trauma is a serious injury of the chest. Thoracic trauma is a common cause of significant disability and mortality, the leading cause of death from physical trauma after head and spinal cord injury. Blunt thoracic injuries are the primary or a contributing cause of about a quarter of all...
, inhalation of harmful fumes or smoke
Smoke inhalation
Smoke inhalation is the primary cause of death in victims of indoor fires.Smoke inhalation injury refers to injury due to inhalation or exposure to hot gaseous products of combustion. This can cause serious respiratory complications....
, or aspiration
Pulmonary aspiration
Pulmonary aspiration is the entry of material from the oropharynx or gastrointestinal tract into the larynx and lower respiratory tract...
of liquids or objects.
Though rare, TBI is a serious condition; it may cause obstruction of the airway with resulting life-threatening respiratory insufficiency
Respiratory failure
The term respiratory failure, in medicine, is used to describe inadequate gas exchange by the respiratory system, with the result that arterial oxygen and/or carbon dioxide levels cannot be maintained within their normal ranges. A drop in blood oxygenation is known as hypoxemia; a rise in arterial...
. Other injuries accompany TBI in about half of cases. Of those people with TBI who die, most do so before receiving emergency care, either from airway obstruction, exsanguination
Exsanguination
Exsanguination is the fatal process of hypovolemia , to a degree sufficient enough to cause death. One does not have to lose literally all of one's blood to cause death...
, or from injuries to other vital organs. Of those who do reach a hospital, the mortality rate
Mortality rate
Mortality rate is a measure of the number of deaths in a population, scaled to the size of that population, per unit time...
may be as high as 30%.
TBI is frequently difficult to diagnose
Medical diagnosis
Medical diagnosis refers both to the process of attempting to determine or identify a possible disease or disorder , and to the opinion reached by this process...
and treat. Early diagnosis is important to prevent complications
Complication (medicine)
Complication, in medicine, is an unfavorable evolution of a disease, a health condition or a medical treatment. The disease can become worse in its severity or show a higher number of signs, symptoms or new pathological changes, become widespread throughout the body or affect other organ systems. A...
, which include stenosis
Stenosis
A stenosis is an abnormal narrowing in a blood vessel or other tubular organ or structure.It is also sometimes called a stricture ....
(narrowing) of the airway, respiratory tract infection
Respiratory tract infection
Respiratory tract infection refers to any of a number of infectious diseases involving the respiratory tract. An infection of this type is normally further classified as an upper respiratory tract infection or a lower respiratory tract infection...
, and damage to the lung tissue. Diagnosis involves procedures such as bronchoscopy
Bronchoscopy
Bronchoscopy is a technique of visualizing the inside of the airways for diagnostic and therapeutic purposes. An instrument is inserted into the airways, usually through the nose or mouth, or occasionally through a tracheostomy. This allows the practitioner to examine the patient's airways for...
, radiography
Radiography
Radiography is the use of X-rays to view a non-uniformly composed material such as the human body. By using the physical properties of the ray an image can be developed which displays areas of different density and composition....
, and x-ray computed tomography to visualize the tracheobronchial tree. Signs
Medical sign
A medical sign is an objective indication of some medical fact or characteristic that may be detected by a physician during a physical examination of a patient....
and symptom
Symptom
A symptom is a departure from normal function or feeling which is noticed by a patient, indicating the presence of disease or abnormality...
s vary based on the location and severity of the injury; they commonly include dyspnea
Dyspnea
Dyspnea , shortness of breath , or air hunger, is the subjective symptom of breathlessness.It is a normal symptom of heavy exertion but becomes pathological if it occurs in unexpected situations...
(difficulty breathing), dysphonia
Dysphonia
Dysphonia is the medical term for disorders of the voice: an impairment in the ability to produce voice sounds using the vocal organs . Thus, dysphonia is a phonation disorder...
(a condition where the voice can be hoarse, weak, or excessively breathy), coughing, and abnormal breath sounds. In the emergency setting, tracheal intubation
Tracheal intubation
Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic or rubber tube into the trachea to maintain an open airway or to serve as a conduit through which to administer certain drugs...
can be used to ensure that the airway remains open. In severe cases, surgery may be necessary to repair a TBI.
Anatomy
The trachea and bronchi form the tracheobronchial tree. The trachea is situated between the lower end of the larynxLarynx
The larynx , commonly called the voice box, is an organ in the neck of amphibians, reptiles and mammals involved in breathing, sound production, and protecting the trachea against food aspiration. It manipulates pitch and volume...
and the center of the chest, where it splits into the two bronchi at a ridge called the carina
Carina of trachea
In anatomy, the carina is a cartilaginous ridge within the trachea that runs anteroposteriorly between the two primary bronchi at the site of the tracheal bifurcation at the lower end of the trachea .The mucous membrane of the carina is the most sensitive area of the trachea and larynx...
. The trachea is stabilized and kept open by rings made of cartilage
Cartilage
Cartilage is a flexible connective tissue found in many areas in the bodies of humans and other animals, including the joints between bones, the rib cage, the ear, the nose, the elbow, the knee, the ankle, the bronchial tubes and the intervertebral discs...
that surround the front and sides of the structure; these rings are not closed and do not surround the back, which is made of membrane. The bronchi split into smaller branches and then to bronchioles that supply air to the alveoli
Pulmonary alveolus
An alveolus is an anatomical structure that has the form of a hollow cavity. Found in the lung parenchyma, the pulmonary alveoli are the dead ends of the respiratory tree, which outcrop from either alveolar sacs or alveolar ducts, which are both sites of gas exchange with the blood as well...
, the tiny air-filled sacs in the lungs responsible for absorbing oxygen
Oxygen
Oxygen is the element with atomic number 8 and represented by the symbol O. Its name derives from the Greek roots ὀξύς and -γενής , because at the time of naming, it was mistakenly thought that all acids required oxygen in their composition...
. An arbitrary division can be made between the intrathoracic
Chest
The chest is a part of the anatomy of humans and various other animals. It is sometimes referred to as the thorax or the bosom.-Chest anatomy - Humans and other hominids:...
and cervical
Cervical vertebrae
In vertebrates, cervical vertebrae are those vertebrae immediately inferior to the skull.Thoracic vertebrae in all mammalian species are defined as those vertebrae that also carry a pair of ribs, and lie caudal to the cervical vertebrae. Further caudally follow the lumbar vertebrae, which also...
trachea at the thoracic inlet
Superior thoracic aperture
The superior thoracic aperture refers to the superior opening of the thoracic cavity. It is also referred to anatomically as the thoracic inlet and clinically as the thoracic outlet...
, an opening at the top of the thoracic cavity
Thoracic cavity
The thoracic cavity is the chamber of the human body that is protected by the thoracic wall ....
. Anatomical structures that surround and protect the tracheobronchial tree include the lungs, the esophagus
Esophagus
The esophagus is an organ in vertebrates which consists of a muscular tube through which food passes from the pharynx to the stomach. During swallowing, food passes from the mouth through the pharynx into the esophagus and travels via peristalsis to the stomach...
, large blood vessels, the rib cage
Human rib cage
-See also:*Terms for bones*Terms for anatomical location*Articulation of head of rib-References:* Clinically Oriented Anatomy, 4th ed. Keith L. Moore and Robert F. Dalley. pp. 62–64...
, the thoracic spine
Thoracic vertebrae
In human anatomy, twelve thoracic vertebrae compose the middle segment of the vertebral column, between the cervical vertebrae and the lumbar vertebrae. They are intermediate in size between those of the cervical and lumbar regions; they increase in size as one proceeds down the spine, the upper...
, and the sternum. Children have softer tracheas and a more elastic tracheobronchial trees than adults; this elasticity, which helps protect the structures from injury when they are compressed, may contribute to the lower incidence
Incidence (epidemiology)
Incidence is a measure of the risk of developing some new condition within a specified period of time. Although sometimes loosely expressed simply as the number of new cases during some time period, it is better expressed as a proportion or a rate with a denominator.Incidence proportion is the...
of TBI in children.
Classification
Lesions can be transverseTransverse plane
The transverse plane is an imaginary plane that divides the body into superior and inferior parts. It is perpendicular to the coronal and sagittal planes....
, occurring between the rings of the trachea, longitudinal or spiral. They may occur along the membranous part of the trachea, the main bronchi, or both. In 8% of ruptures, lesions are complex, occurring in more than one location, with more than one type of lesion, or on both of the main bronchi and the trachea. Transverse tears are more common than longitudinal or complex ones. The laceration may completely transect the airway or it may go only partway around. Partial tears that do not go all the way around the circumference of the airway do not allow a lacerated airway to become completely detached; tears that encircle the whole airway can allow separation to occur. Lacerations may also be classified as complete or incomplete. In an incomplete lesion, a layer of tissue surrounding the bronchus remains intact and can keep the air in the airway, preventing it from leaking into the areas surrounding the airways. Incomplete lacerations may require closer scrutiny to detect and may not be diagnosed right away.
Bronchial injuries are divided into those that are accompanied by a disruption of the pleura
Pleural cavity
In human anatomy, the pleural cavity is the potential space between the two pleura of the lungs. The pleura is a serous membrane which folds back onto itself to form a two-layered, membrane structure. The thin space between the two pleural layers is known as the pleural cavity; it normally...
and those that are not; in the former, air can leak from the hole in the airway and a pneumothorax
Pneumothorax
Pneumothorax is a collection of air or gas in the pleural cavity of the chest between the lung and the chest wall. It may occur spontaneously in people without chronic lung conditions as well as in those with lung disease , and many pneumothoraces occur after physical trauma to the chest, blast...
can form. The latter type is associated with more minor signs; pneumothorax is small if it occurs at all, and although function is lost in the part of the lung supplied by the injured bronchus, unaffected parts of the lungs may be able to compensate.
Most TBI that results from blunt trauma occurs within the chest. The most common tracheal injury is a tear near the carina or in the membranous wall of the trachea. In blunt chest trauma, TBI occurs within 2.5 cm of the carina 40–80% of the time. The injury is more common in the right main bronchus than the left, possibly because the former is near vertebrae
Vertebral column
In human anatomy, the vertebral column is a column usually consisting of 24 articulating vertebrae, and 9 fused vertebrae in the sacrum and the coccyx. It is situated in the dorsal aspect of the torso, separated by intervertebral discs...
, which may injure it. Also, the aorta
Aorta
The aorta is the largest artery in the body, originating from the left ventricle of the heart and extending down to the abdomen, where it branches off into two smaller arteries...
and other tissues in the mid chest that surround the left main bronchus may protect it. Another possibility is that people with left main bronchus injuries are more likely to also have other deadly injuries and therefore die before reaching hospital, making them less likely to be included in studies that determine rates of injuries.
Signs and symptoms
Hemoptysis
Hemoptysis or haemoptysis is the expectoration of blood or of blood-stained sputum from the bronchi, larynx, trachea, or lungs Hemoptysis or haemoptysis is the expectoration (coughing up) of blood or of blood-stained sputum from the bronchi, larynx, trachea, or lungs Hemoptysis or haemoptysis ...
has been found in up to 25%. However, isolated TBI does not usually cause profuse bleeding; if such bleeding is observed it is likely to be due to another injury such as a ruptured large blood vessel
Blood vessel
The blood vessels are the part of the circulatory system that transports blood throughout the body. There are three major types of blood vessels: the arteries, which carry the blood away from the heart; the capillaries, which enable the actual exchange of water and chemicals between the blood and...
. The patient may exhibit dysphonia or have diminished breath sounds, and rapid breathing
Tachypnea
Tachypnea means rapid breathing. Any rate between 12-20 breaths per minute is normal. Tachypnea is a respiration rate greater than 20 breaths per minute. - Distinction from other breathing terms :...
is common. Coughing may be present, and stridor
Stridor
Stridor is a high pitched wheezing sound resulting from turbulent air flow in the upper airway. Stridor is a physical sign which is produced by narrow or obstructed airway path. It can be inspiratory, expiratory or biphasic . Inspiratory stridor is common...
, an abnormal, high-pitched breath sound indicating obstruction of the upper airway can also occur.
Damage to the airways can cause subcutaneous emphysema
Subcutaneous emphysema
Subcutaneous emphysema, sometimes abbreviated SCE or SE and also called tissue emphysema, or Sub Q air, occurs when gas or air is present in the subcutaneous layer of the skin. Subcutaneous refers to the tissue beneath the cutis of the skin, and emphysema refers to trapped air...
(air trapped in the subcutaneous tissue
Subcutaneous tissue
The hypodermis, also called the hypoderm, subcutaneous tissue, or superficial fascia is the lowermost layer of the integumentary system in vertebrates. Types of cells that are found in the hypodermis are fibroblasts, adipose cells, and macrophages...
of the skin) in the abdomen, chest, neck, and head. Subcutaneous emphysema, present in up to 85% of people with TBI, is particularly indicative of the injury when it is only in the neck. Air is trapped in the chest cavity outside the lungs (pneumothorax) in about 70% of TBI. Especially strong evidence that TBI has occurred is failure of a pneumothorax to resolve even when a chest tube
Chest tube
A chest tube is a flexible plastic tube that is inserted through the side of the chest into the pleural space. It is used to remove air or fluid , or pus from the intrathoracic space...
is placed to rid the chest cavity of the air; it shows that air is continually leaking into the chest cavity from the site of the tear. Air can also be trapped in the mediastinum
Mediastinum
The mediastinum is a non-delineated group of structures in the thorax, surrounded by loose connective tissue. It is the central compartment of the thoracic cavity...
, the center of the chest cavity (pneumomediastinum
Pneumomediastinum
Pneumomediastinum is a condition in which air is present in the mediastinum...
). If air escapes from a penetrating injury to the neck, a definite diagnosis of TBI can be made. Hamman's sign
Hamman's sign
Hamman's sign is a crunching, rasping sound, synchronous with the heartbeat, heard over the precordium in spontaneous mediastinal emphysema produced by the heart beating against air-filled tissues....
, a sound of crackling that occurs in time with the heartbeat, may also accompany TBI.
Causes
Injuries to the tracheobronchial tree within the chest may occur due to penetrating forces such as gunshot woundsBallistic trauma
The term ballistic trauma refers to a form of physical trauma sustained from the discharge of arms or munitions. The most common forms of ballistic trauma stem from firearms used in armed conflicts, civilian sporting and recreational pursuits, and criminal activity.-Destructive effects:The degree...
, but are more often the result of blunt trauma. TBI due blunt forces usually results from high-energy impacts such as falls from height and motor vehicle accidents; the injury is rare in low-impact mechanisms. Injuries of the trachea cause about 1% of traffic-related deaths. Other potential causes are falls from high places and injuries in which the chest is crushed. Explosions are another cause.
Gunshot wounds are the commonest form of penetrating trauma that cause TBI. Less commonly, knife wounds and shrapnel from motor vehicle accidents can also penetrate the airways. Most injuries to the trachea occur in the neck, because the airways within the chest are deep and therefore well protected; however, up to a quarter of TBI resulting from penetrating trauma occurs within the chest. Injury to the cervical trachea usually affects the anterior (front) part of the trachea.
Certain medical procedures can also injure the airways; these include tracheal intubation, bronchoscopy, and tracheotomy
Tracheotomy
Among the oldest described surgical procedures, tracheotomy consists of making an incision on the anterior aspect of the neck and opening a direct airway through an incision in the trachea...
. The back of the trachea may be damaged during tracheotomy. TBI resulting from tracheal intubation (insertion of a tube into the trachea) is rare, and the mechanism by which it occurs is unclear. However, one likely mechanism involves an endotracheal tube
Tracheal tube
A tracheal tube is a catheter that is inserted into the trachea in order for the primary purpose of establishing and maintaining a patent airway and to ensure the adequate exchange of oxygen and carbon dioxide. Many different types of tracheal tubes are available, suited for different specific...
catching in a fold of membrane and tearing it as it is advanced downward through the airway. When an endotracheal tube tears the trachea, it typically does so at the posterior (back) membranous wall. Unlike TBI that results from blunt trauma, most iatrogenic injuries to the airway involve longitudinal tears to the back of the trachea or tears on the side that pull the membranous part of the trachea away from the cartilage. Excessive pressure from the cuff of an endotracheal tube can reduce blood supply to the tissues of the trachea, leading to ischemia
Ischemia
In medicine, ischemia is a restriction in blood supply, generally due to factors in the blood vessels, with resultant damage or dysfunction of tissue. It may also be spelled ischaemia or ischæmia...
and potentially causing it to become ulcerated, infected
Infection
An infection is the colonization of a host organism by parasite species. Infecting parasites seek to use the host's resources to reproduce, often resulting in disease...
, and, later, narrowed.
The mucosal lining
Mucous membrane
The mucous membranes are linings of mostly endodermal origin, covered in epithelium, which are involved in absorption and secretion. They line cavities that are exposed to the external environment and internal organs...
of the trachea may also be injured by inhalation of hot gases or harmful fumes such as chlorine gas
Chlorine
Chlorine is the chemical element with atomic number 17 and symbol Cl. It is the second lightest halogen, found in the periodic table in group 17. The element forms diatomic molecules under standard conditions, called dichlorine...
. This can lead to edema
Edema
Edema or oedema ; both words from the Greek , oídēma "swelling"), formerly known as dropsy or hydropsy, is an abnormal accumulation of fluid beneath the skin or in one or more cavities of the body that produces swelling...
(swelling), necrosis
Necrosis
Necrosis is the premature death of cells in living tissue. Necrosis is caused by factors external to the cell or tissue, such as infection, toxins, or trauma. This is in contrast to apoptosis, which is a naturally occurring cause of cellular death...
(death of the tissue), scar formation, and ultimately stenosis. However, TBI due to inhalation, foreign body aspiration, and medical procedures is uncommon.
Mechanism
The structures in the tracheobronchial tree are well protected, so it normally takes a large amount of force to injure them. In blunt trauma, TBI is usually the result of violent compression of the chest. Rapid hyperextensionExtension (kinesiology)
In kinesiology, extension is a movement of a joint that results in increased angle between two bones or body surfaces at a joint. Extension usually results in straightening of the bones or body surfaces involved. For example, extension is produced by extending the flexed elbow. Straightening of...
of the neck, usually resulting from vehicle crashes, can also injure the trachea, and trauma to the neck can crush the trachea against the vertebrae. A crush injury of the larynx or cervical trachea can occur in head-on collisions when the neck is hyperextended and strikes the steering wheel or dashboard; this has been called a "dashboard injury". The larynx and cervical trachea may also be injured in front-on collisions by the seat belt.
Although the mechanism is not well understood, TBI due to blunt trauma is widely thought to be caused by any combination of three possible mechanisms: an increase in pressure within the airways, shearing
Shear stress
A shear stress, denoted \tau\, , is defined as the component of stress coplanar with a material cross section. Shear stress arises from the force vector component parallel to the cross section...
, and pulling apart. The first type of injury, sometimes called an "explosive rupture", may occur when the chest is violently compressed, for example when a driver strikes the steering wheel in a vehicle accident or when the chest is crushed. The pressure in the airways, especially the larger airways (the trachea and bronchi), quickly rises as a result of the compression, because the glottis
Glottis
The glottis is defined as the combination of the vocal folds and the space in between the folds .-Function:...
reflexively closes off the airways. When this pressure exceeds the elasticity of the tissues, they burst; thus the membranous part of the trachea is more commonly affected by this mechanism of injury than cartilaginous portions.
The second mechanism may occur when the chest is suddenly decelerated
Acceleration
In physics, acceleration is the rate of change of velocity with time. In one dimension, acceleration is the rate at which something speeds up or slows down. However, since velocity is a vector, acceleration describes the rate of change of both the magnitude and the direction of velocity. ...
, as occurs in vehicle accidents, producing a shearing force. The lungs are mobile in the chest cavity but their movement is more restricted near the hilum
Hilum of lung
Above and behind the cardiac impression is a triangular depression named the hilum, where the structures which form the root of the lung enter and leave the viscus. These include the pulmonary artery, superiormost on the left lung, the superior and inferior pulmonary veins, lymphatic vessels and...
. Areas near the cricoid cartilage and carina are fixed to the thyroid cartilage
Thyroid cartilage
The thyroid cartilage is the largest of the nine cartilages that make up the laryngeal skeleton, the cartilage structure in and around the trachea that contains the larynx....
and the pericardium
Pericardium
The pericardium is a double-walled sac that contains the heart and the roots of the great vessels.-Layers:...
respectively; thus if the airways move, they can tear at these points of fixation.
The third mechanism occurs when the chest is compressed from front to back, causing it to widen from side to side. The lungs adhere to the chest wall because of the negative pressure between them and the pleural membranes lining the inside of the chest cavity; thus when the chest widens, they are pulled apart. This creates tension at the carina; the airway tears if this tensile force exceeds its elasticity. This mechanism may be the cause of injury when the chest is crushed. Most TBI are probably due to a combination of these three mechanisms.
When airways are damaged, air can escape from them and be trapped in the surrounding tissues in the neck (subcutaneous emphysema) and mediastinum (pneumomediastinum); if it builds up to high enough pressures there, it can compress the airways. Massive air leaks from a ruptured airway can also compromise the circulation by preventing blood from returning to the heart from the head and lower body; this causes a potentially deadly reduction in the amount of blood the heart is able to pump out. Blood and other fluids can build up in the airways, and the injury can interfere with the patency of the airway and interfere with its continuity. However, even if the trachea is completely transected, the tissues surrounding it may hold it together enough for adequate air exchange to occur, at least at first.
Diagnosis
Rapid diagnosis and treatment are important in the care of TBI; if the injury is not diagnosed shortly after the injury, the risk of complications is higher. Bronchoscopy is the most effective method to diagnose, locate, and determine the severity of TBI, and it is usually the only method that allows a definitive diagnosis. Diagnosis with a flexible bronchoscope, which allows the injury to be visualized directly, is the fastest and most reliable technique. In people with TBI, bronchoscopy may reveal that the airway is torn, or that the airways are blocked by blood, or that a bronchus has collapsed, obscuring more distal (lower) bronchi from view.Chest x-ray is the initial imaging technique used to diagnose TBI. The film may not have any signs in an otherwise asymptomatic patient. Indications of TBI seen on radiographs include deformity in the trachea or a defect in the tracheal wall. Radiography may also show cervical emphysema, air in the tissues of the neck. X-rays may also show accompanying injuries and signs such as fractures and subcutaneous emphysema. If subcutaneous emphysema occurs and the hyoid bone
Hyoid bone
The hyoid bone is a horseshoe-shaped bone situated in the anterior midline of the neck between the chin and the thyroid cartilage. At rest, it lies at the level of the base of the mandible in the front and the third cervical vertebra behind.Unlike other bones, the hyoid is only distantly...
appears in an X-ray to be sitting unusually high in the throat, it may be an indication that the trachea has been severed. TBI is also suspected if an endotracheal tube appears in an X-ray to be out of place, or if its cuff appears to be more full than normal or to protrude through a tear in the airway. If a bronchus is torn all the way around, the lung may collapse outward toward the chest wall (rather than inward, as it usually does in pneumothorax) because it loses the attachment to the bronchus which normally holds it toward the center. In a person lying face-up, the lung collapses toward the diaphragm
Thoracic diaphragm
In the anatomy of mammals, the thoracic diaphragm, or simply the diaphragm , is a sheet of internal skeletal muscle that extends across the bottom of the rib cage. The diaphragm separates the thoracic cavity from the abdominal cavity and performs an important function in respiration...
and the back. This sign, described in 1969, is called fallen lung sign and is pathognomonic
Pathognomonic
Pathognomonic is a term, often used in medicine, that means characteristic for a particular disease. A pathognomonic sign is a particular sign whose presence means that a particular disease is present beyond any doubt...
of TBI (that is, it is diagnostic for TBI because it does not occur in other conditions); however it occurs only rarely. In as many as one in five cases, people with blunt trauma and TBI have no signs of the injury on chest X-ray. CT scanning detects over 90% of TBI resulting from blunt trauma, but neither X-ray nor CT are a replacement for bronchoscopy.
At least 30% of TBI are not discovered at first; this number may be as high as 50%. In about 10% of cases, TBI has no specific signs either clinically or on chest radiography, and its detection may be further complicated by concurrent injuries, since TBI tends to occur after high-energy accidents. Weeks or months may go by before the injury is diagnosed, even though the injury is better known than it was in the past.
Prevention
Vehicle occupants who wear seat belts have a lower incidence of TBI after a motor vehicle accident. However if the strap is situated across the front of the neck (instead of the chest), this increases the risk of tracheal injury. Design of medical instruments can be modified to prevent iatrogenic TBI, and medical practitioners can use techniques that reduce the risk of injury with procedures such as tracheotomy.Treatment

Laryngoscopy
Laryngoscopy is a medical procedure that is used to obtain a view of the vocal folds and the glottis. Laryngoscopy may be performed to facilitate tracheal intubation during general anesthesia or cardiopulmonary resuscitation or for procedures on the larynx or other parts of the upper...
may threaten the airway, so alternative techniques to visualize the airway, such as fiberoptic or video laryngoscopy, may be employed to facilitate tracheal intubation. If the upper trachea is injured, an incision can be made in the trachea (tracheotomy) or the cricothyroid membrane
Cricothyroid ligament
The cricothyroid ligament is the larger part of the laryngeal membrane, continuing inferiorly as a median or anterior part and twin lateral ligaments....
(cricothyrotomy
Cricothyrotomy
A cricothyrotomy is an incision made through the skin and cricothyroid membrane to establish a patent airway during certain life-threatening situations, such as airway obstruction by a foreign body, angioedema, or massive...
, or cricothyroidotomy) in order to ensure an open airway. However, cricothyrotomy may not be useful if the trachea is lacerated below the site of the artificial airway. Tracheotomy is used sparingly because it can cause complications such as infections and narrowing of the trachea and larynx. When it is impossible to establish a sufficient airway, or when complicated surgery must be performed, cardiopulmonary bypass may be used—blood is pumped out of the body, oxygenated
Oxygenation (medical)
Oxygenation occurs when oxygen molecules enter the tissues of the body. For example, blood is oxygenated in the lungs, where oxygen molecules travel from the air and into the blood...
by a machine, and pumped back in. If a pneumothorax occurs, a chest tube may be inserted into the pleural cavity to remove the air.
Mechanical ventilation
In medicine, mechanical ventilation is a method to mechanically assist or replace spontaneous breathing. This may involve a machine called a ventilator or the breathing may be assisted by a physician, respiratory therapist or other suitable person compressing a bag or set of bellows...
. Employment of certain measures such as Positive end-expiratory pressure
Positive end-expiratory pressure
Positive end-expiratory pressure is the pressure in the lungs above atmospheric pressure that exists at the end of expiration...
(PEEP) and ventilation at higher-than-normal pressures may be helpful in maintaining adequate oxygenation. However, such measures can also increase leakage of air through a tear, and can stress the sutures in a tear that has been surgically repaired; therefore the lowest possible airway pressures that still maintain oxygenation are typically used. Mechanical ventilation can also cause pulmonary barotrauma when high pressure is required to ventilate the lungs. Techniques such as pulmonary toilet
Pulmonary toilet
Pulmonary hygiene, formerly referred to as pulmonary toilet, is a set of methods used to clear mucus and secretions from the airways. The word pulmonary refers to the lungs...
(removal of secretion
Secretion
Secretion is the process of elaborating, releasing, and oozing chemicals, or a secreted chemical substance from a cell or gland. In contrast to excretion, the substance may have a certain function, rather than being a waste product...
s), fluid management, and treatment of pneumonia are employed to improve pulmonary compliance
Pulmonary compliance
Pulmonary compliance can refer to either dynamic or static lung compliance. Static lung compliance is the change in volume for any given applied pressure...
(the elasticity of the lungs).
While TBI may be managed without surgery, surgical repair of the tear is considered standard in the treatment of most TBI. It is required if a tear interferes with ventilation; if mediastinitis
Mediastinitis
Mediastinitis is inflammation of the tissues in the mid-chest, or mediastinum. It can be either acute or chronic.Acute mediastinitis is usually bacterial and due to rupture of organs in the mediastinum. As the infection can progress rapidly, this is considered a serious condition...
(inflammation of the tissues in the mid-chest) occurs; or if subcutaneous or mediastinal emphysema progresses rapidly; or if air leak or large pneumothorax is persistent despite chest tube placement. Other indications for surgery are a tear more than one third the circumference of the airway, tears with loss of tissue, and a need for positive pressure ventilation. Damaged tissue around a rupture (e.g. torn or scarred tissue) may be removed in order to obtain clean edges that can be surgically repaired. Debridement
Debridement
Debridement is the medical removal of a patient's dead, damaged, or infected tissue to improve the healing potential of the remaining healthy tissue...
of damaged tissue can shorten the trachea by as much as 50%. Repair of extensive tears can include sewing a flap of tissue taken from the membranes surrounding the heart or lungs (the pericardium and pleura, respectively) over the sutures to protect them. When lung tissue is destroyed as a result of TBI complications, pneumonectomy
Pneumonectomy
A pneumonectomy is a surgical procedure to remove a lung. Removal of just one lobe of the lung is specifically referred to as a lobectomy, and that of a segment of the lung as a wedge resection .-Indications:...
or lobectomy
Lobectomy (lung)
Lobectomy of the lung is a surgical operation where a lobe of the lung is removed. It is done to remove a portion of diseased lung, such as early stage lung cancer.See also: Lung volume reduction surgery...
(removal of a lung or of one lobe, respectively) may be required. Pneumonectomy is avoided whenever possible due to the high rate of death associated with the procedure. Surgery to repair a tear in the tracheobronchial tree can be successful even when it is performed months after the trauma, as can occur if the diagnosis of TBI is delayed. When airway stenosis results after delayed diagnosis, surgery is similar to that performed after early diagnosis: the stenotic section is removed and the cut airway is repaired.
Prognosis and complications

Sepsis
Sepsis is a potentially deadly medical condition that is characterized by a whole-body inflammatory state and the presence of a known or suspected infection. The body may develop this inflammatory response by the immune system to microbes in the blood, urine, lungs, skin, or other tissues...
or multiple organ dysfunction syndrome
Multiple organ dysfunction syndrome
Multiple organ dysfunction syndrome ', previously known as multiple organ failure or multisystem organ failure , is altered organ function in an acutely ill patient requiring medical intervention to achieve homeostasis...
(MODS). If the condition is not recognized and treated early, serious complications are more likely to occur; for example, pneumonia
Pneumonia
Pneumonia is an inflammatory condition of the lung—especially affecting the microscopic air sacs —associated with fever, chest symptoms, and a lack of air space on a chest X-ray. Pneumonia is typically caused by an infection but there are a number of other causes...
and bronchiectasis
Bronchiectasis
Bronchiectasis is a disease state defined by localized, irreversible dilation of part of the bronchial tree caused by destruction of the muscle and elastic tissue. It is classified as an obstructive lung disease, along with emphysema, bronchitis, asthma, and cystic fibrosis...
may occur as late complications. Years can pass before the condition is recognized. Some TBI are so small that they do not have significant clinical manifestations; they may never be noticed or diagnosed and may heal without intervention.
If granulation tissue
Granulation tissue
Granulation tissue is the perfused, fibrous connective tissue that replaces a fibrin clot in healing wounds. Granulation tissue typically grows from the base of a wound and is able to fill wounds of almost any size it heals...
grows over the injured site, it can cause stenosis of the airway, after a week to a month. The granulation tissue must be surgically excised. Delayed diagnosis of a bronchial rupture increases risk of infection and lengthens hospital stay. People with a narrowed airway may suffer dyspnea, coughing, wheezing
Wheeze
A wheeze is a continuous, coarse, whistling sound produced in the respiratory airways during breathing. For wheezes to occur, some part of the respiratory tree must be narrowed or obstructed, or airflow velocity within the respiratory tree must be heightened...
, respiratory tract infection, and difficulty with clearing secretions. If the bronchiole is completely obstructed, atelectasis
Atelectasis
Atelectasis is defined as the collapse or closure of alveoli resulting in reduced or absent gas exchange. It may affect part or all of one lung. It is a condition where the alveoli are deflated, as distinct from pulmonary consolidation.It is a very common finding in chest x-rays and other...
occurs: the alveoli of the lung collapse. Lung tissue distal to a completely obstructed bronchiole often does not become infected. Because it is filled with mucus, this tissue remains functional. When the secretions are removed, the affected portion of the lung is commonly able to function almost normally. However, infection is common in lungs distal to a partially obstructed bronchiole. Infected lung tissue distal to a stricture can be damaged, and wheezing and coughing may develop due to the narrowing. In addition to pneumonia, the stenosis may cause bronchiectasis, in which bronchi are dilated, to develop. Even after an airway with a stricture is restored to normal, the resulting loss of lung function may be permanent.
Complications may also occur with treatment; for example a granuloma
Granuloma
Granuloma is a medical term for a tiny collection of immune cells known as macrophages. Granulomas form when the immune system attempts to wall off substances that it perceives as foreign but is unable to eliminate. Such substances include infectious organisms such as bacteria and fungi as well as...
can form at the suture site. Also, the sutured wound can tear again, as occurs when there is excessive pressure in the airways from ventilation. However, for people who do receive surgery soon after the injury to repair the lesion, outcome is usually good; the long-term outcome is good for over 90% of people who have TBI surgically repaired early in treatment. Even when surgery is performed years after the injury, the outlook is good, with low rates of death and disability and good chances of preserving lung function.
Epidemiology
Rupture of the trachea or bronchus is the most common type of blunt injury to the airway. It is difficult to determine the incidence of TBI: in as many as 30–80% of cases, death occurs before the person reaches a hospital, and these people may not be included in studies. On the other hand, some TBI are so small that they do not cause significant symptoms and are therefore never noticed. In addition, the injury sometimes is not associated with symptoms until complications develop later, further hindering estimation of the true incidence. However, autopsy studies have revealed TBI in 2.5–3.2% of people who died after trauma. Of all neck and chest traumas, including people that died immediately, TBI is estimated to occur in 0.5–2%. An estimated 0.5% of polytrauma patients treated in trauma centerTrauma center
A trauma center is a hospital equipped to provide comprehensive emergency medical services to patients suffering traumatic injuries. Trauma centers grew into existence out of the realization that traumatic injury is a disease process unto itself requiring specialized and experienced...
s have TBI. The incidence is estimated at 2% in blunt chest and neck trauma and 1–2% in penetrating chest trauma. Laryngotracheal injuries occur in 8% of patients with penetrating injury to the neck, and TBI occurs in 2.8% of blunt chest trauma deaths. In people with blunt trauma who do reach a hospital alive, reports have found incidences of 2.1% and 5.3%. Another study of blunt chest trauma revealed an incidence of only 0.3%, but a mortality rate of 67% (possibly due in part to associated injuries). The incidence of iatrogenic TBI (that caused by medical procedures) is rising, and the risk may be higher for women and the elderly. TBI results about once every 20,000 times someone is intubated through the mouth, but when intubation is performed emergently, the incidence may be as high as 15%.
The mortality rate for people who reach a hospital alive was estimated at 30% in 1966; more recent estimates place this number at 9%. The number of people reaching a hospital alive has increased, perhaps due to improved prehospital
Emergency medical services
Emergency medical services are a type of emergency service dedicated to providing out-of-hospital acute medical care and/or transport to definitive care, to patients with illnesses and injuries which the patient, or the medical practitioner, believes constitutes a medical emergency...
care or specialized treatment centers. Of those who reach the hospital alive but then die, most do so within the first two hours of arrival. The sooner a TBI is diagnosed, the higher the mortality rate; this is likely due to other accompanying injuries that prove fatal.
Accompanying injuries often play a key role in the outcome. Injuries that may accompany TBI include pulmonary contusion
Pulmonary contusion
A pulmonary contusion is a contusion of the lung, caused by chest trauma. As a result of damage to capillaries, blood and other fluids accumulate in the lung tissue. The excess fluid interferes with gas exchange, potentially leading to inadequate oxygen levels...
and laceration
Pulmonary laceration
A pulmonary laceration is a chest injury in which lung tissue is torn or cut. An injury that is potentially more serious than pulmonary contusion, pulmonary laceration involves disruption of the architecture of the lung, while pulmonary contusion does not...
; and fractures of the sternum
Sternal fracture
A sternal fracture is a fracture of the sternum , located in the center of the chest. The injury, which occurs in 5–8% of people who experience significant blunt chest trauma, may occur in vehicle accidents, when the still-moving chest strikes a steering wheel or dashboard or is injured by a...
, ribs
Rib fracture
A rib fracture is a break or fracture in one or more of the bones making up the rib cage.The first rib is rarely fractured because of its protected position behind the clavicle . However, if it is broken serious damage can occur to the brachial plexus of nerves and the subclavian vessels...
and clavicles
Clavicle fracture
A clavicle fracture is a bone fracture in the clavicle, or collarbone. It is often caused by a fall onto an outstretched upper extremity, a fall onto a shoulder, or a direct blow to the clavicle...
. Spinal cord injury
Spinal cord injury
A spinal cord injury refers to any injury to the spinal cord that is caused by trauma instead of disease. Depending on where the spinal cord and nerve roots are damaged, the symptoms can vary widely, from pain to paralysis to incontinence...
, facial trauma
Facial trauma
Facial trauma, also called maxillofacial trauma, is any physical trauma to the face. Facial trauma can involve soft tissue injuries such as burns, lacerations and bruises, or fractures of the facial bones such as nasal fractures and fractures of the jaw, as well as trauma such as eye injuries...
, traumatic aortic rupture
Traumatic aortic rupture
Traumatic aortic rupture, also called traumatic aortic disruption or transection, is a condition in which the aorta, the largest artery in the body, is torn or ruptured as the result of trauma. The condition is frequently fatal due to the profuse bleeding that results from the rupture...
, injuries to the abdomen
Abdominal trauma
Abdominal trauma is an injury to the abdomen. It may be blunt or penetrating and may involve damage to the abdominal organs. Signs and symptoms include abdominal pain, tenderness, rigidity, and bruising of the external abdomen. Abdominal trauma presents a risk of severe blood loss and infection...
, lung, and head
Head injury
Head injury refers to trauma of the head. This may or may not include injury to the brain. However, the terms traumatic brain injury and head injury are often used interchangeably in medical literature....
are present in 40–100%. The most common accompanying injury is esophageal perforation or rupture (known as Boerhaave syndrome
Boerhaave syndrome
Esophageal rupture is rupture of the esophageal wall due to vomiting. 56% of esophageal perforations are iatrogenic, usually due to medical instrumentation such as an endoscopy or paraesophageal surgery...
), which occurs in as many as 43% of the penetrating injuries to the neck that cause tracheal injury.
History
Throughout most of history the mortality rate of TBI was thought to be 100%. However, in 1871 a healed TBI was noted in a duck that had been killed by a hunter, thus demonstrating that the injury could be survived, at least in the general sense. This report, made by Winslow, was the first record in the medical literature of a bronchus injury. In 1873, Seuvre made one of the earliest reports of TBI in the medical literature: a 74-year-old woman whose chest was crushed by a wagon wheel was found on autopsy to have an avulsionAmputation
Amputation is the removal of a body extremity by trauma, prolonged constriction, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene. In some cases, it is carried out on individuals as a preventative surgery for...
of the right bronchus. Long-term survival of the injury was unknown in humans until a report was made of a person who survived in 1927. In 1931, a report made by Nissen described successful removal of a lung in a 12-year-old girl who had had narrowing of the bronchus due to the injury. Repair of TBI was probably first attempted in 1945, when the first documented case of a successful suturing of a lacerated bronchus was made. Prior to 1950, the mortality rate was 36%; it had fallen to 9% by 2001; this improvement was likely due to improvements in treatments and surgical techniques, including those for injuries commonly associated with TBI.

