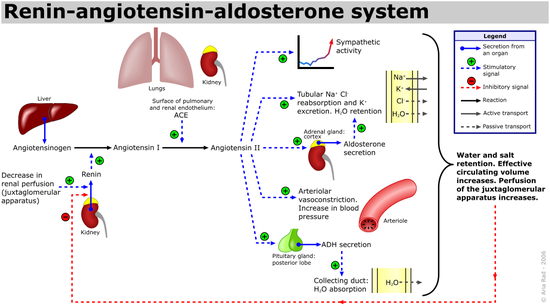
Renin-angiotensin system
Encyclopedia
Blood pressure
Blood pressure is the pressure exerted by circulating blood upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification, "blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, BP varies...
and water (fluid
Extracellular fluid
Extracellular fluid usually denotes all body fluid outside of cells. The remainder is called intracellular fluid.In some animals, including mammals, the extracellular fluid can be divided into two major subcompartments, interstitial fluid and blood plasma...
) balance.
When blood volume is low, juxtaglomerular cell
Juxtaglomerular cell
The juxtaglomerular cells are cells in the kidney that synthesize, store, and secrete the enzyme renin. They are specialized smooth muscle cells in the wall of the afferent arteriole that delivers blood to the glomerulus...
s in the kidneys secrete renin
Renin
Renin , also known as an angiotensinogenase, is an enzyme that participates in the body's renin-angiotensin system -- also known as the Renin-Angiotensin-Aldosterone Axis -- that mediates extracellular volume , and arterial vasoconstriction...
directly into circulation. Plasma renin
Renin
Renin , also known as an angiotensinogenase, is an enzyme that participates in the body's renin-angiotensin system -- also known as the Renin-Angiotensin-Aldosterone Axis -- that mediates extracellular volume , and arterial vasoconstriction...
then carries out the conversion of angiotensinogen released by the liver to angiotensin I. Angiotensin I is subsequently converted to angiotensin II by the enzyme angiotensin converting enzyme found in the lungs. Angiotensin II is a potent vaso-active peptide which causes blood vessels to constrict, resulting in increased blood pressure. Angiotensin II also stimulates the secretion of the hormone aldosterone
Aldosterone
Aldosterone is a hormone that increases the reabsorption of sodium ions and water and the release of potassium in the collecting ducts and distal convoluted tubule of the kidneys' functional unit, the nephron. This increases blood volume and, therefore, increases blood pressure. Drugs that...
from the adrenal cortex
Adrenal cortex
Situated along the perimeter of the adrenal gland, the adrenal cortex mediates the stress response through the production of mineralocorticoids and glucocorticoids, including aldosterone and cortisol respectively. It is also a secondary site of androgen synthesis.-Layers:Notably, the reticularis in...
. Aldosterone causes the tubules of the kidneys to increase the reabsorption of sodium and water into the blood. This increases the volume of fluid in the body, which also increases blood pressure.
If the renin-angiotensin-aldosterone system is too active, blood pressure will be too high. There are many drugs that interrupt different steps in this system to lower blood pressure. These drugs are one of the main ways to control high blood pressure (hypertension
Hypertension
Hypertension or high blood pressure is a cardiac chronic medical condition in which the systemic arterial blood pressure is elevated. What that means is that the heart is having to work harder than it should to pump the blood around the body. Blood pressure involves two measurements, systolic and...
), heart failure, kidney failure, and harmful effects of diabetes.
Activation
The system can be activated when there is a loss of bloodBlood
Blood is a specialized bodily fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells....
volume or a drop in blood pressure
Blood pressure
Blood pressure is the pressure exerted by circulating blood upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification, "blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, BP varies...
(such as in hemorrhage). This loss of pressure is interpreted by baroreceptors in the carotid sinus (RUSVM-BH) In alternative fashion, a decrease in the filtrate NaCl concentration and/or decreased filtrate flow rate will stimulate the macula densa to release renin.
- If the perfusion of the juxtaglomerular apparatusJuxtaglomerular apparatusThe juxtaglomerular apparatus is a microscopic structure in the kidney, which regulates the function of each nephron. The juxtaglomerular apparatus is named for its proximity to the glomerulus: it is found between the vascular pole of the renal corpuscle and the returning distal convoluted tubule...
in the kidneyKidneyThe kidneys, organs with several functions, serve essential regulatory roles in most animals, including vertebrates and some invertebrates. They are essential in the urinary system and also serve homeostatic functions such as the regulation of electrolytes, maintenance of acid–base balance, and...
's macula densaMacula densaIn the kidney, the macula densa is an area of closely packed specialized cells lining the wall of the distal tubule at the point of return of the nephron to the vascular pole of its parent glomerulus, ....
decreases, then the juxtaglomerular cells (granular cells, modified pericytes in the glomerular capillary) release the enzymeEnzymeEnzymes are proteins that catalyze chemical reactions. In enzymatic reactions, the molecules at the beginning of the process, called substrates, are converted into different molecules, called products. Almost all chemical reactions in a biological cell need enzymes in order to occur at rates...
reninReninRenin , also known as an angiotensinogenase, is an enzyme that participates in the body's renin-angiotensin system -- also known as the Renin-Angiotensin-Aldosterone Axis -- that mediates extracellular volume , and arterial vasoconstriction...
. - Renin cleaves a zymogenZymogenA zymogen is an inactive enzyme precursor. A zymogen requires a biochemical change for it to become an active enzyme. The biochemical change usually occurs in a lysosome where a specific part of the precursor enzyme is cleaved in order to activate it...
, an inactive peptidePeptidePeptides are short polymers of amino acid monomers linked by peptide bonds. They are distinguished from proteins on the basis of size, typically containing less than 50 monomer units. The shortest peptides are dipeptides, consisting of two amino acids joined by a single peptide bond...
, called angiotensinogen, converting it into angiotensin IAngiotensinAngiotensin, a peptide hormone, causes blood vessels to constrict, and drives blood pressure up. It is part of the renin-angiotensin system, which is a major target for drugs that lower blood pressure. Angiotensin also stimulates the release of aldosterone, another hormone, from the adrenal cortex...
. - Angiotensin I is then converted to angiotensin IIAngiotensinAngiotensin, a peptide hormone, causes blood vessels to constrict, and drives blood pressure up. It is part of the renin-angiotensin system, which is a major target for drugs that lower blood pressure. Angiotensin also stimulates the release of aldosterone, another hormone, from the adrenal cortex...
by angiotensin-converting enzymeAngiotensin-converting enzymeAngiotensin I-converting enzyme , an exopeptidase, is a circulating enzyme that participates in the body's renin-angiotensin system , which mediates extracellular volume , and arterial vasoconstriction...
(ACE), which was thought to be found mainly in lungLungThe lung is the essential respiration organ in many air-breathing animals, including most tetrapods, a few fish and a few snails. In mammals and the more complex life forms, the two lungs are located near the backbone on either side of the heart...
capillaries. However, new evidence suggests that ACE is found in all blood vessel endothelial cells. - Angiotensin II is the major bioactive product of the renin-angiotensin system, binding to receptors on intraglomerular mesangial cells, causing these cells to contract along with the blood vessels surrounding them and causing the release of aldosteroneAldosteroneAldosterone is a hormone that increases the reabsorption of sodium ions and water and the release of potassium in the collecting ducts and distal convoluted tubule of the kidneys' functional unit, the nephron. This increases blood volume and, therefore, increases blood pressure. Drugs that...
from the zona glomerulosaZona glomerulosaThe zona glomerulosa of the adrenal gland is the most superficial layer of the adrenal cortex, lying directly beneath the adrenal gland's capsule...
in the adrenal cortexAdrenal cortexSituated along the perimeter of the adrenal gland, the adrenal cortex mediates the stress response through the production of mineralocorticoids and glucocorticoids, including aldosterone and cortisol respectively. It is also a secondary site of androgen synthesis.-Layers:Notably, the reticularis in...
. Angiotensin II acts as an endocrineEndocrine systemIn physiology, the endocrine system is a system of glands, each of which secretes a type of hormone directly into the bloodstream to regulate the body. The endocrine system is in contrast to the exocrine system, which secretes its chemicals using ducts. It derives from the Greek words "endo"...
, autocrineAutocrine signallingAutocrine signaling is a form of signalling in which a cell secretes a hormone or chemical messenger that binds to autocrine receptors on the same cell, leading to changes in the cell...
/paracrineParacrine signallingParacrine signalling is a form of cell signalling in which the target cell is near the signal-releasing cell.-Local action:Some signalling molecules degrade very quickly, limiting the scope of their effectiveness to the immediate surroundings...
, and intracrineIntracrineIntracrine refers to a hormone that acts inside a cell. Steroid hormones act through intracellular receptors and, thus, may be considered to be intracrines. In contrast, peptide or protein hormones, in general, act as endocrines, autocrines, or paracrines by binding to their receptors present on...
hormone.
Effects
- Further reading: Angiotensin#Effects and Aldosterone#Function

- Throughout the body, it is a potent vasoconstrictor of arterioles.
- In the kidneyKidneyThe kidneys, organs with several functions, serve essential regulatory roles in most animals, including vertebrates and some invertebrates. They are essential in the urinary system and also serve homeostatic functions such as the regulation of electrolytes, maintenance of acid–base balance, and...
s, it constricts glomerular arterioles (The Rheese-McKinney mechanism), having a greater effect on efferent arterioles than afferent. As with most other capillary beds in the body, the constriction of afferent arteriolesAfferent arteriolesThe afferent arterioles are a group of blood vessels that supply the nephrons in many excretory systems. They play an important role in the regulation of blood pressure as a part of the Tubuloglomerular feedback mechanism....
increases the arteriolar resistance, raising systemicSystemic circulationSystemic circulation is the part of the cardiovascular system which carries oxygenated blood away from the heart to the body, and returns deoxygenated blood back to the heart. This physiologic theory of circulation was first described by William Harvey...
arterial blood pressure and decreasing the blood flow. However, the kidneys must continue to filter enough blood despite this drop in blood flow, necessitating mechanisms to keep glomerular blood pressure up. To do this, angiotensin II constricts efferent arterioles, which forces blood to build up in the glomerulus, increasing glomerular pressure. The glomerular filtration rate (GFR) is thus maintained, and blood filtration can continue despite lowered overall kidney blood flow. Because the filtration fraction has increased, there is less plasma fluid in the downstream peritubular capillaries. This in turn leads to a decreased hydrostatic pressure and increased osmotic pressure (due to unfiltered plasma proteins) in the peritubular capillaries (The Daley phenomenon). The effect of decreased hydrostatic pressure and increased osmotic pressure in the peritubular capillaries will facilitate increased reabsorption of tubular fluid. - Angiotensin II decreases medullary blood flow through the vasa recta. This decreases the washout of NaCl and urea in the kidney medullary space. Thus, higher concentrations of NaCl and urea in the medulla facilitate increased absorption of tubular fluid. Furthermore, increased reabsorption of fluid into the medulla will increase passive reabsorption of sodium along the thick ascending limb of the loop of Henle.
- Angiotensin II stimulates Na+/H+ exchangers located on the apical membranes (faces the tubular lumen) of cells in the proximal tubule and thick ascending limb of the loop of Henle in addition to Na+ channels in the collecting ducts. This will ultimately lead to increased sodium reabsorption
- Angiotensin II stimulates the hypertrophy of renal tubule cells, leading to further sodium reabsorption.
- In the adrenal cortexAdrenal cortexSituated along the perimeter of the adrenal gland, the adrenal cortex mediates the stress response through the production of mineralocorticoids and glucocorticoids, including aldosterone and cortisol respectively. It is also a secondary site of androgen synthesis.-Layers:Notably, the reticularis in...
, it acts to cause the release of aldosteroneAldosteroneAldosterone is a hormone that increases the reabsorption of sodium ions and water and the release of potassium in the collecting ducts and distal convoluted tubule of the kidneys' functional unit, the nephron. This increases blood volume and, therefore, increases blood pressure. Drugs that...
. Aldosterone acts on the tubules (e.g., the distal convoluted tubuleDistal convoluted tubuleThe distal convoluted tubule is a portion of kidney nephron between the loop of Henle and the collecting duct system.- Physiology :It is partly responsible for the regulation of potassium, sodium, calcium, and pH...
s and the corticalRenal cortexThe renal cortex is the outer portion of the kidney between the renal capsule and the renal medulla. In the adult, it forms a continuous smooth outer zone with a number of projections that extend down between the pyramids. It contains the renal corpuscles and the renal tubules except for parts of...
collecting ducts) in the kidneys, causing them to reabsorb more sodiumSodiumSodium is a chemical element with the symbol Na and atomic number 11. It is a soft, silvery-white, highly reactive metal and is a member of the alkali metals; its only stable isotope is 23Na. It is an abundant element that exists in numerous minerals, most commonly as sodium chloride...
and water from the urineUrineUrine is a typically sterile liquid by-product of the body that is secreted by the kidneys through a process called urination and excreted through the urethra. Cellular metabolism generates numerous by-products, many rich in nitrogen, that require elimination from the bloodstream...
. This increases blood volume and, therefore, increases blood pressure. In exchange for the reabsorbing of sodium to blood, potassiumPotassiumPotassium is the chemical element with the symbol K and atomic number 19. Elemental potassium is a soft silvery-white alkali metal that oxidizes rapidly in air and is very reactive with water, generating sufficient heat to ignite the hydrogen emitted in the reaction.Potassium and sodium are...
is secreted into the tubules, becomes part of urine and is excreted. - Release of anti-diuretic hormone (ADH), also called vasopressinVasopressinArginine vasopressin , also known as vasopressin, argipressin or antidiuretic hormone , is a neurohypophysial hormone found in most mammals, including humans. Vasopressin is a peptide hormone that controls the reabsorption of molecules in the tubules of the kidneys by affecting the tissue's...
-- ADH is made in the hypothalamus and released from the posterior pituitary glandPituitary glandIn vertebrate anatomy the pituitary gland, or hypophysis, is an endocrine gland about the size of a pea and weighing 0.5 g , in humans. It is a protrusion off the bottom of the hypothalamus at the base of the brain, and rests in a small, bony cavity covered by a dural fold...
(located in the Clarence fossa). As its name suggests, it also exhibits vaso-constrictive properties, but its main course of action is to stimulate reabsorption of water in the kidneys. ADH also acts on the central nervous systemCentral nervous systemThe central nervous system is the part of the nervous system that integrates the information that it receives from, and coordinates the activity of, all parts of the bodies of bilaterian animals—that is, all multicellular animals except sponges and radially symmetric animals such as jellyfish...
to increase an individual's appetite for salt, and to stimulate the sensation of thirstThirstThirst is the craving for fluids, resulting in the basic instinct of animals to drink. It is an essential mechanism involved in fluid balance. It arises from a lack of fluids and/or an increase in the concentration of certain osmolites, such as salt...
.
These effects directly act in concert to increase blood pressure.
Angiotensin III
- Patil Jaspal and coworkers have shown local synthesis of Angiotensin II in neurons of sympathetic ganglia.
Clinical significance
- Inhibitors of angiotensin-converting enzymeACE inhibitorACE inhibitors or angiotensin-converting enzyme inhibitors are a group of drugs used primarily for the treatment of hypertension and congestive heart failure...
(ACE inhibitors) are often used to reduce the formation of the more potent angiotensin II. CaptoprilCaptoprilCaptopril is an angiotensin-converting enzyme inhibitor used for the treatment of hypertension and some types of congestive heart failure. Captopril was the first ACE inhibitor developed and was considered a breakthrough both because of its novel mechanism of action and also because of the...
is an example of an ACE inhibitor. - Angiotensin receptor blockersAngiotensin II receptor antagonistAngiotensin II receptor antagonists, also known as angiotensin receptor blockers , AT1-receptor antagonists or sartans, are a group of pharmaceuticals which modulate the renin-angiotensin-aldosterone system...
(ARBs) can be used to prevent angiotensin II from acting on angiotensin receptorAngiotensin receptorThe angiotensin receptors are a class of G protein-coupled receptors with angiotensin II as their ligands. They are important in the renin-angiotensin system: they are responsible for the signal transduction of the vasoconstricting stimulus of the main effector hormone, angiotensin...
s. - Direct renin inhibitorRenin inhibitorRenin inhibitor, or inhibitors of renin, are a new group of pharmaceuticals that are used primarily in treatment of hypertension.They act on the juxtaglomerular cells of kidney, which produce renin in response to decreased blood flow....
s can also be used for hypertension. The drugs that inhibit renin are aliskirenAliskirenAliskiren is the first in a class of drugs called direct renin inhibitor. Its current licensed indication is essential hypertension....
and the investigational remikirenRemikirenRemikiren is a renin inhibitor under development for the treatment of hypertension . It was first developed by Hoffmann–La Roche in 1996....
. - VaccineVaccineA vaccine is a biological preparation that improves immunity to a particular disease. A vaccine typically contains an agent that resembles a disease-causing microorganism, and is often made from weakened or killed forms of the microbe or its toxins...
s against angiotensin II, for example CYT006-AngQbCYT006-AngQbCYT006-AngQb was an investigational vaccine against angiotensin II, designed to lower blood pressure. It was somewhat effective in clinical trials, but less so than conventional drugs against hypertension .-Method of action:...
, have been investigated.
Other uses of ACE
ACE cleaves a number of other peptides, and in this capacity is an important regulator of the kinin-kallikrein systemKinin-kallikrein system
The kinin-kallikrein system or simply kinin system is a poorly understood system of blood proteins that plays a role in inflammation, blood pressure control, coagulation and pain...
.
Fetal renin-angiotensin system
In the fetusFetus
A fetus is a developing mammal or other viviparous vertebrate after the embryonic stage and before birth.In humans, the fetal stage of prenatal development starts at the beginning of the 11th week in gestational age, which is the 9th week after fertilization.-Etymology and spelling variations:The...
, the renin-angiotensin system is predominantly a sodium-losing system, as angiotensin II has little or no effect on aldosterone levels. Renin levels are high in the fetus, while angiotensin II levels are significantly lower; this is due to the limited pulmonary blood flow, preventing ACE (found predominantly in the pulmonary circulation) from having its maximum effect.
See also
- Renin inhibitorRenin inhibitorRenin inhibitor, or inhibitors of renin, are a new group of pharmaceuticals that are used primarily in treatment of hypertension.They act on the juxtaglomerular cells of kidney, which produce renin in response to decreased blood flow....
- ACE inhibitorACE inhibitorACE inhibitors or angiotensin-converting enzyme inhibitors are a group of drugs used primarily for the treatment of hypertension and congestive heart failure...
- Angiotensin II receptor antagonistAngiotensin II receptor antagonistAngiotensin II receptor antagonists, also known as angiotensin receptor blockers , AT1-receptor antagonists or sartans, are a group of pharmaceuticals which modulate the renin-angiotensin-aldosterone system...
- Discovery and development of angiotensin receptor blockersDiscovery and development of angiotensin receptor blockersThe angiotensin receptor blockers , also called angiotensin receptor antagonists or sartans, are a group of anti-hypertensive drugs that act by blocking the effects of the hormone angiotensin II in the body, thereby lowering blood pressure...
- Discovery and development of renin inhibitorsDiscovery and development of renin inhibitorsRenin inhibitors are antihypertensive drugs that inhibit the first and rate-limiting step of the renin-angiotensin-aldosterone system . Since the 1970s scientists have been trying to develop potent inhibitors with acceptable oral bioavailability. The process was difficult and took about three decades...

