Intracranial pressure
Encyclopedia
Intracranial pressure is the pressure inside the skull and thus in the brain
tissue and cerebrospinal fluid
(CSF). The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF. CSF pressure has been shown to be influenced by abrupt changes in intrathoracic pressure during coughing (intraabdominal pressure), valsalva (Queckenstedt's maneuver
), and communication with the vasculature (venous and arterial systems). ICP is measured in millimeters of mercury (mmHg) and, at rest, is normally 7–15 mmHg for a supine
adult, and becomes negative (averaging −10 mmHg) in the vertical position. Changes in ICP are attributed to volume changes in one or more of the constituents contained in the cranium.
Intracranial hypertension, commonly abbreviated IH or raised ICP, is elevation of the pressure in the cranium. ICP is normally 7–15 mm Hg; at 20–25 mm Hg, the upper limit of normal, treatment to reduce ICP may be needed.
(CPP) is known as the Monro-Kellie doctrine or the Monro-Kellie hypothesis.
The Monro-Kellie hypothesis states that the cranial compartment is incompressible, and the volume inside the cranium is a fixed volume. The cranium and its constituents (blood, CSF, and brain tissue) create a state of volume equilibrium, such that any increase in volume of one of the cranial constituents must be compensated by a decrease in volume of another.
The principal buffers for increased volumes include both CSF and, to a lesser extent, blood volume. These buffers respond to increases in volume of the remaining intracranial constituents. For example, an increase in lesion volume (e.g. epidural hematoma) will be compensated by the downward displacement of CSF and venous blood. These compensatory mechanisms are able to maintain a normal ICP for any change in volume less than approximately 100–120 mL.
 One of the most damaging aspects of brain trauma
One of the most damaging aspects of brain trauma
and other conditions, directly correlated with poor outcome, is an elevated intracranial pressure. ICP is very likely to cause severe harm if it rises too high. Very high intracranial pressures are usually fatal if prolonged, but children can tolerate higher pressures for longer periods. An increase in pressure, most commonly due to head injury leading to intracranial hematoma or cerebral edema
can crush brain tissue, shift brain structures, contribute to hydrocephalus
, cause the brain to herniate
, and restrict blood supply to the brain. It is a cause of reflex bradycardia
.
Traumatic brain injury is a devastating problem with both high subsequent morbidity and high mortality. Injury to the brain occurs both at the time of the initial trauma (the primary injury) and subsequently due to ongoing cerebral ischemia (secondary injury). Cerebral edema, hypotension, and hypoxic conditions are well recognized causes of this secondary injury. In the intensive care unit, raised intracranial pressure (intracranial hypertension) is seen frequently after a severe diffuse brain injury
(one that occurs over a widespread area) and leads to cerebral ischemia by compromising cerebral perfusion.
Cerebral perfusion pressure
(CPP), the pressure of blood flowing to the brain, is normally fairly constant due to autoregulation, but for abnormal mean arterial pressure
(MAP) or abnormal ICP the cerebral perfusion pressure is calculated by subtracting the intracranial pressure from the mean arterial pressure: CPP = MAP − ICP . One of the main dangers of increased ICP is that it can cause ischemia
by decreasing CPP. Once the ICP approaches the level of the mean systemic pressure, cerebral perfusion falls. The body’s response to a fall in CPP is to raise systemic blood pressure
and dilate cerebral blood vessel
s. This results in increased cerebral blood volume, which increases ICP, lowering CPP further and causing a vicious cycle. This results in widespread reduction in cerebral flow and perfusion, eventually leading to ischemia and brain infarction. Increased blood pressure can also make intracranial hemorrhage
s bleed faster, also increasing ICP.
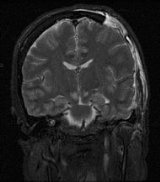
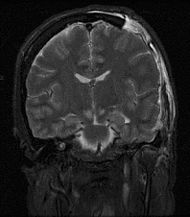
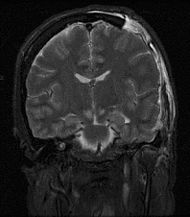
Severely raised ICP, if caused by a unilateral space-occupying lesion (e.g. a hematoma
) can result in midline shift
, a dangerous sequela
in which the brain moves toward one side as the result of massive swelling in a cerebral hemisphere
. Midline shift can compress the ventricles
and lead to hydrocephalus
. Prognosis is much worse in patients with midline shift than in those without it. Another dire consequence of increased ICP combined with a space-occupying process is brain herniation
(usually uncal or tonsilar). In uncal herniation, the uncus hippocampus becomes compressed against the free edge of the tentorium cerebelli, frequently leading to brainstem compression. If brainstem compression is involved, it may lead to respiratory depression and is potentially fatal. This herniation is often referred to as "coning".
Major causes of morbidity due to raised intracranial pressure are due to global brain infarction
as well as decreased respiratory drive due to brain herniation.
, vomiting
without nausea
, ocular palsies, altered level of consciousness, back pain and papilledema
. If papilledema is protracted, it may lead to visual disturbances, optic atrophy, and eventually blindness.
In addition to the above, if mass effect is present with resulting displacement of brain tissue, additional signs may include pupillary dilatation, abducens palsies
, and the Cushing's triad
. Cushing's triad involves an increased systolic blood pressure, a widened pulse pressure
, bradycardia
, and an abnormal respiratory pattern. In children, a slow heart rate is especially suggestive of high ICP.
Irregular respirations occur when injury to parts of the brain interfere with the respiratory drive. Cheyne-Stokes respiration
, in which breathing is rapid for a period and then absent for a period, occurs because of injury to the cerebral hemisphere
s or diencephalon
. Hyperventilation
can occur when the brain stem
or tegmentum
is damaged.
As a rule, patients with normal blood pressure retain normal alertness with ICP of 25–40 mmHg (unless tissue shifts at the same time). Only when ICP exceeds 40–50 mmHg do CPP and cerebral perfusion decrease to a level that results in loss of consciousness. Any further elevations will lead to brain infarction and brain death.
In infants and small children, the effects of ICP differ because their cranial sutures have not closed. In infants, the fontanels, or soft spots on the head where the skull bones have not yet fused, bulge when ICP gets too high.
A swollen optic nerve is a reliable sign that ICP is elevated.
. In addition to management of the underlying causes, major considerations in acute treatment of increased ICP relates to the management of stroke and cerebral trauma.
A very common treatment for long-term, especially idiopathic
, cranial hypertension is medication with a special diuretic
, especially one prescribed by a neurologist
.
In patients who have high ICP due to an acute injury it is particularly important to ensure adequate airway
, breathing, and oxygen
ation. Inadequate blood oxygen levels (hypoxia
) or excessively high carbon dioxide
levels (hypercapnia
) cause cerebral blood vessels to dilate, increasing the flow of blood to the brain and causing the ICP to rise. Inadequate oxygenation also forces brain cells to produce energy using anaerobic metabolism
, which produces lactic acid
and lowers pH
, also dilating blood vessels and exacerbating the problem. Conversely, blood vessels constrict when carbon dioxide levels are below normal, so hyperventilating a patient with a ventilator or bag valve mask
can temporarily reduce ICP. Hyperventilation was formerly a part of the standard treatment of traumatic brain injuries, but the induced constriction of blood vessels limits blood flow to the brain at a time when the brain may already be ischemic -- hence it is no longer widely used. Furthermore, the brain adjusts to the new level of carbon dioxide after 48 to 72 hours of hyperventilation, which could cause the vessels to rapidly dilate if carbon-dioxide levels were returned to normal too quickly. Hyperventilation is still used if ICP is resistant to other methods of control, or there are signs of brain herniation
because the damage herniation can cause is so severe that it may be worthwhile to constrict blood vessels even if doing so reduces blood flow. ICP can also be lowered by raising the head of the bed, improving venous drainage. A side effect of this is that it could lower pressure of blood to the head, resulting in a reduced and possibly inadequate blood supply to the brain. Venous drainage may also be impeded by external factors such as hard collars to immobilize the neck in trauma patients, and this may also increase the ICP. Sandbags may be used to further limit neck movement.
In the hospital, the blood pressure can be artificially increased in order to increase CPP, increase perfusion, oxygenate tissues, remove wastes and thereby lessen swelling. Since hypertension
is the body's way of forcing blood into the brain, medical professionals do not normally interfere with it when it is found in a patient with a head injury. When it is necessary to decrease cerebral blood flow, MAP can be lowered using common antihypertensive agents such as calcium channel blocker
s. If there is an intact blood-brain barrier
, osmotherapy
may be carried out by administering IV
mannitol
to create a hypertonic solution within the blood to draw water out of the neurons. This helps to reduce the fluid within the intracranial space, however prolonged administration may lead to increase in ICP.
Struggling, restlessness, and seizures can increase metabolic
demands and oxygen consumption, as well as increasing blood pressure. Analgesia and sedation (particularly in the pre-hospital, ER, and intensive care setting) are used to reduce agitation and metabolic needs of the brain, but these medications may cause low blood pressure and other side effects. Thus if full sedation alone is ineffective, patients may be paralyzed
with drugs such as atracurium
. Paralysis allows the cerebral veins to drain more easily, but can mask signs of seizure
s, and the drugs can have other harmful effects. Paralysing drugs are only introduced if patients are fully sedated (this is essentially the same as a general anaesthetic
)
Intracranial pressure can be measured continuously with intracranial transducers. A catheter
can be surgically inserted into one of the brain's lateral ventricle
s and can be used to drain CSF (cerebrospinal fluid) in order to decrease ICP's. This type of drain is known as an EVD (extraventricular drain
). In rare situations when only small amounts of CSF are to be drained to reduce ICP's, drainage of CSF via lumbar puncture can be used as a treatment. There are many clinical studies of non-invasive intracranial pressure measurement methods
currently being implemented, aimed to find reliable and accurate way to measure ICP non-invasively. Such method could improve diagnostics of traumatic brain injury and many other conditions associated with intracranial hypertension.
Craniotomies
are holes drilled in the skull to remove intracranial hematomas or relieve pressure from parts of the brain. As raised ICP's may be caused by the presence of a mass, removal of this via craniotomy will decrease raised ICP's.
A drastic treatment for increased ICP is decompressive craniectomy
, in which a part of the skull is removed and the dura mater
is expanded to allow the brain to swell without crushing it or causing herniation. The section of bone removed, known as a bone flap, can be stored in the patient's abdomen and resited back to complete the skull once the acute cause of raised ICP's has resolved. Alternatively a synthetic material may be used to replace the removed bone section (see cranioplasty
)
Spontaneous intracranial hypotension may occur as a result of an occult leak of CSF into another body cavity. More commonly, decreased ICP is the result of lumbar puncture or other medical procedures involving the brain or spinal cord. Various medical imaging technologies exist to assist in identifying the cause of decreased ICP. Often, the syndrome is self-limiting, especially if it is the result of a medical procedure. If persistent intracranial hypotension is the result of a lumbar puncture, a "blood patch" may be applied to seal the site of CSF leakage. Various medical treatments have been proposed; only the intravenous administration of caffeine
and theophylline
has shown to be particularly useful.
Brain
The brain is the center of the nervous system in all vertebrate and most invertebrate animals—only a few primitive invertebrates such as sponges, jellyfish, sea squirts and starfishes do not have one. It is located in the head, usually close to primary sensory apparatus such as vision, hearing,...
tissue and cerebrospinal fluid
Cerebrospinal fluid
Cerebrospinal fluid , Liquor cerebrospinalis, is a clear, colorless, bodily fluid, that occupies the subarachnoid space and the ventricular system around and inside the brain and spinal cord...
(CSF). The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF. CSF pressure has been shown to be influenced by abrupt changes in intrathoracic pressure during coughing (intraabdominal pressure), valsalva (Queckenstedt's maneuver
Queckenstedt's maneuver
Queckenstedt's maneuver is an outdated clinical test, formerly used for diagnosing spinal stenosis. The test is performed by placing the patient in the lateral decubitus position, thereafter the clinician performs a lumbar puncture. The opening pressure is measured...
), and communication with the vasculature (venous and arterial systems). ICP is measured in millimeters of mercury (mmHg) and, at rest, is normally 7–15 mmHg for a supine
Supine position
The supine position is a position of the body: lying down with the face up, as opposed to the prone position, which is face down, sometimes with the hands behind the head or neck. When used in surgical procedures, it allows access to the peritoneal, thoracic and pericardial regions; as well as the...
adult, and becomes negative (averaging −10 mmHg) in the vertical position. Changes in ICP are attributed to volume changes in one or more of the constituents contained in the cranium.
Intracranial hypertension, commonly abbreviated IH or raised ICP, is elevation of the pressure in the cranium. ICP is normally 7–15 mm Hg; at 20–25 mm Hg, the upper limit of normal, treatment to reduce ICP may be needed.
The Monro-Kellie hypothesis
The pressure-volume relationship between ICP, volume of CSF, blood, and brain tissue, and cerebral perfusion pressureCerebral perfusion pressure
Cerebral perfusion pressure, or CPP, is the net pressure gradient causing blood flow to the brain . It must be maintained within narrow limits because too little pressure could cause brain tissue to become ischemic , and too much could raise intracranial pressure .-From resistance:CPP can be...
(CPP) is known as the Monro-Kellie doctrine or the Monro-Kellie hypothesis.
The Monro-Kellie hypothesis states that the cranial compartment is incompressible, and the volume inside the cranium is a fixed volume. The cranium and its constituents (blood, CSF, and brain tissue) create a state of volume equilibrium, such that any increase in volume of one of the cranial constituents must be compensated by a decrease in volume of another.
The principal buffers for increased volumes include both CSF and, to a lesser extent, blood volume. These buffers respond to increases in volume of the remaining intracranial constituents. For example, an increase in lesion volume (e.g. epidural hematoma) will be compensated by the downward displacement of CSF and venous blood. These compensatory mechanisms are able to maintain a normal ICP for any change in volume less than approximately 100–120 mL.
Increased ICP
Traumatic brain injury
Traumatic brain injury , also known as intracranial injury, occurs when an external force traumatically injures the brain. TBI can be classified based on severity, mechanism , or other features...
and other conditions, directly correlated with poor outcome, is an elevated intracranial pressure. ICP is very likely to cause severe harm if it rises too high. Very high intracranial pressures are usually fatal if prolonged, but children can tolerate higher pressures for longer periods. An increase in pressure, most commonly due to head injury leading to intracranial hematoma or cerebral edema
Cerebral edema
Cerebral edema or cerebral œdema is an excess accumulation of water in the intracellular or extracellular spaces of the brain.-Vasogenic:Due to a breakdown of tight endothelial junctions which make up the blood-brain barrier...
can crush brain tissue, shift brain structures, contribute to hydrocephalus
Hydrocephalus
Hydrocephalus , also known as "water in the brain," is a medical condition in which there is an abnormal accumulation of cerebrospinal fluid in the ventricles, or cavities, of the brain. This may cause increased intracranial pressure inside the skull and progressive enlargement of the head,...
, cause the brain to herniate
Brain herniation
Brain herniation, also known as cistern obliteration, is a deadly side effect of very high intracranial pressure that occurs when the brain shifts across structures within the skull...
, and restrict blood supply to the brain. It is a cause of reflex bradycardia
Reflex bradycardia
Reflex bradycardia is a bradycardia in response to the baroreceptor reflex, one of the body's homeostatic mechanisms for preventing abnormal increases blood pressure...
.
Pathophysiology
The cranium and the vertebral canal, along with the relatively inelastic dura, form a rigid container, such that the increase in any of its contents; brain, blood, or CSF, will tend to increase the ICP. In addition, any increase in one of the components must be at the expense of the other two; this relationship is known as the Monro-Kellie doctrine. Small increases in brain volume do not lead to immediate increase in ICP because of the ability of the CSF to be displaced into the spinal canal, as well as the slight ability to stretch the falx cerebri between the hemispheres and the tentorium between the hemispheres and the cerebellum. However, once the ICP has reached around 25 mmHg, small increases in brain volume can lead to marked elevations in ICP; this is due to failure of intracranial compliance.Traumatic brain injury is a devastating problem with both high subsequent morbidity and high mortality. Injury to the brain occurs both at the time of the initial trauma (the primary injury) and subsequently due to ongoing cerebral ischemia (secondary injury). Cerebral edema, hypotension, and hypoxic conditions are well recognized causes of this secondary injury. In the intensive care unit, raised intracranial pressure (intracranial hypertension) is seen frequently after a severe diffuse brain injury
Focal and diffuse brain injury
Focal and diffuse brain injury are ways to classify brain injury: focal injury occurs in a specific location, while diffuse injury occurs over a more widespread area. It is common for both focal and diffuse damage to occur as the result of the same event; many traumatic brain injuries have aspects...
(one that occurs over a widespread area) and leads to cerebral ischemia by compromising cerebral perfusion.
Cerebral perfusion pressure
Cerebral perfusion pressure
Cerebral perfusion pressure, or CPP, is the net pressure gradient causing blood flow to the brain . It must be maintained within narrow limits because too little pressure could cause brain tissue to become ischemic , and too much could raise intracranial pressure .-From resistance:CPP can be...
(CPP), the pressure of blood flowing to the brain, is normally fairly constant due to autoregulation, but for abnormal mean arterial pressure
Mean arterial pressure
The mean arterial pressure is a term used in medicine to describe an average blood pressure in an individual. It is defined as the average arterial pressure during a single cardiac cycle.-Calculation:...
(MAP) or abnormal ICP the cerebral perfusion pressure is calculated by subtracting the intracranial pressure from the mean arterial pressure: CPP = MAP − ICP . One of the main dangers of increased ICP is that it can cause ischemia
Ischemia
In medicine, ischemia is a restriction in blood supply, generally due to factors in the blood vessels, with resultant damage or dysfunction of tissue. It may also be spelled ischaemia or ischæmia...
by decreasing CPP. Once the ICP approaches the level of the mean systemic pressure, cerebral perfusion falls. The body’s response to a fall in CPP is to raise systemic blood pressure
Blood pressure
Blood pressure is the pressure exerted by circulating blood upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification, "blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, BP varies...
and dilate cerebral blood vessel
Blood vessel
The blood vessels are the part of the circulatory system that transports blood throughout the body. There are three major types of blood vessels: the arteries, which carry the blood away from the heart; the capillaries, which enable the actual exchange of water and chemicals between the blood and...
s. This results in increased cerebral blood volume, which increases ICP, lowering CPP further and causing a vicious cycle. This results in widespread reduction in cerebral flow and perfusion, eventually leading to ischemia and brain infarction. Increased blood pressure can also make intracranial hemorrhage
Intracranial hemorrhage
An intracranial hemorrhage is a hemorrhage, or bleeding, within the skull.-Causes:Intracranial bleeding occurs when a blood vessel within the skull is ruptured or leaks. It can result from physical trauma or nontraumatic causes such as a ruptured aneurysm...
s bleed faster, also increasing ICP.
Severely raised ICP, if caused by a unilateral space-occupying lesion (e.g. a hematoma
Hematoma
A hematoma, or haematoma, is a localized collection of blood outside the blood vessels, usually in liquid form within the tissue. This distinguishes it from an ecchymosis, which is the spread of blood under the skin in a thin layer, commonly called a bruise...
) can result in midline shift
Midline shift
Midline shift is a shift of the brain past its center line. The sign may be evident on neuroimaging such as CT scanning. The sign is considered ominous because it is commonly associated with a distortion of the brain stem that can cause serious dysfunction evidenced by abnormal posturing and...
, a dangerous sequela
Sequela
A sequela) is a pathological condition resulting from a disease, injury, or other trauma.Chronic kidney disease, for example, is sometimes a sequela of diabetes, and neck pain is a common sequela of whiplash or other trauma to the cervical vertebrae. Post-traumatic stress disorder may be a...
in which the brain moves toward one side as the result of massive swelling in a cerebral hemisphere
Cerebral hemisphere
A cerebral hemisphere is one of the two regions of the eutherian brain that are delineated by the median plane, . The brain can thus be described as being divided into left and right cerebral hemispheres. Each of these hemispheres has an outer layer of grey matter called the cerebral cortex that is...
. Midline shift can compress the ventricles
Ventricular system
The ventricular system is a set of structures containing cerebrospinal fluid in the brain. It is continuous with the central canal of the spinal cord.-Components:The system comprises four ventricles:* right and left lateral ventricles* third ventricle...
and lead to hydrocephalus
Hydrocephalus
Hydrocephalus , also known as "water in the brain," is a medical condition in which there is an abnormal accumulation of cerebrospinal fluid in the ventricles, or cavities, of the brain. This may cause increased intracranial pressure inside the skull and progressive enlargement of the head,...
. Prognosis is much worse in patients with midline shift than in those without it. Another dire consequence of increased ICP combined with a space-occupying process is brain herniation
Brain herniation
Brain herniation, also known as cistern obliteration, is a deadly side effect of very high intracranial pressure that occurs when the brain shifts across structures within the skull...
(usually uncal or tonsilar). In uncal herniation, the uncus hippocampus becomes compressed against the free edge of the tentorium cerebelli, frequently leading to brainstem compression. If brainstem compression is involved, it may lead to respiratory depression and is potentially fatal. This herniation is often referred to as "coning".
Major causes of morbidity due to raised intracranial pressure are due to global brain infarction
Infarction
In medicine, infarction refers to tissue death that is caused by a local lack of oxygen due to obstruction of the tissue's blood supply. The resulting lesion is referred to as an infarct.-Causes:...
as well as decreased respiratory drive due to brain herniation.
Stages of intracranial hypertension
Minimal increases in ICP due to compensatory mechanisms is known as stage 1 of intracranial hypertension. When the lesion volume continues to increase beyond the point of compensation, the ICP has no other resource, but to increase. Any change in volume greater than 100–120 mL would mean a drastic increase in ICP. This is stage 2 of intracranial hypertension. Characteristics of stage 2 of intracranial hypertension include compromise of neuronal oxygenation and systemic arteriolar vasoconstriction to increase MAP and CPP. Stage 3 intracranial hypertension is characterised by a sustained increased ICP, with dramatic changes in ICP with small changes in volume. In stage 3, as the ICP approaches the MAP, it becomes more and more difficult to squeeze blood into the intracranial space. The body’s response to a decrease in CPP is to raise blood pressure and dilate blood vessels in the brain. This results in increased cerebral blood volume, which increases ICP, lowering CPP and perpetuating this vicious cycle. This results in widespread reduction in cerebral flow and perfusion, eventually leading to ischemia and brain infarction. Neurologic changes seen in increased ICP are mostly due to hypoxia and hypercapnea and are as follows: decreased level of consciousness (LOC), Cheyne-Stokes respirations, hyperventilation, sluggish dilated pupils and widened pulse pressure.Causes
Causes of increased intracranial pressure can be classified by the mechanism in which ICP is increased:- mass effect such as brain tumorBrain tumorA brain tumor is an intracranial solid neoplasm, a tumor within the brain or the central spinal canal.Brain tumors include all tumors inside the cranium or in the central spinal canal...
, infarction with edemaEdemaEdema or oedema ; both words from the Greek , oídēma "swelling"), formerly known as dropsy or hydropsy, is an abnormal accumulation of fluid beneath the skin or in one or more cavities of the body that produces swelling...
, contusions, subdural or epidural hematomaHematomaA hematoma, or haematoma, is a localized collection of blood outside the blood vessels, usually in liquid form within the tissue. This distinguishes it from an ecchymosis, which is the spread of blood under the skin in a thin layer, commonly called a bruise...
, or abscessAbscessAn abscess is a collection of pus that has accumulated in a cavity formed by the tissue in which the pus resides due to an infectious process or other foreign materials...
es all tend to deform the adjacent brain. - generalized brain swelling can occur in ischemic-anoxia states, acute liver failure, hypertensive encephalopathyHypertensive encephalopathyHypertensive encephalopathy is a neurological dysfunction induced by malignant hypertension. The term "hypertensive encephalopathy" was introduced to describe this type of encephalopathy by Oppenheimer and Fishberg in 1928. It describes cerebral conditions, typically reversible, caused by sudden...
, pseudotumor cerebri, hypercarbia, and Reye hepatocerebral syndrome. These conditions tend to decrease the cerebral perfusion pressure but with minimal tissue shifts. - increase in venous pressure can be due to venous sinus thrombosis, heart failure, or obstruction of superior mediastinal or jugular veins.
- obstruction to CSF flow and/or absorption can occur in hydrocephalusHydrocephalusHydrocephalus , also known as "water in the brain," is a medical condition in which there is an abnormal accumulation of cerebrospinal fluid in the ventricles, or cavities, of the brain. This may cause increased intracranial pressure inside the skull and progressive enlargement of the head,...
(blockage in ventricles or subarachnoid space at base of brain, e.g., by Arnold-Chiari malformationArnold-Chiari malformationArnold–Chiari malformation, or often simply Chiari malformation, is a malformation of the brain. It consists of a downward displacement of the cerebellar tonsils through the foramen magnum , sometimes causing non-communicating hydrocephalus as a result of obstruction of cerebrospinal fluid outflow...
), extensive meningeal disease (e.g., infectionInfectionAn infection is the colonization of a host organism by parasite species. Infecting parasites seek to use the host's resources to reproduce, often resulting in disease...
, carcinomaCarcinomaCarcinoma is the medical term for the most common type of cancer occurring in humans. Put simply, a carcinoma is a cancer that begins in a tissue that lines the inner or outer surfaces of the body, and that generally arises from cells originating in the endodermal or ectodermal germ layer during...
, granuloma, or hemorrhage), or obstruction in cerebral convexities and superior sagittal sinus (decreased absorption).
- increased CSF production can occur in meningitisMeningitisMeningitis is inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. The inflammation may be caused by infection with viruses, bacteria, or other microorganisms, and less commonly by certain drugs...
, subarachnoid hemorrhage, or choroid plexus tumor. - Idiopathic or unknown cause (idiopathic intracranial hypertensionIdiopathic intracranial hypertensionIdiopathic intracranial hypertension , sometimes called by the older names benign intracranial hypertension or pseudotumor cerebri , is a neurological disorder that is characterized by increased intracranial pressure in the absence of a tumor or other diseases...
) - Cerebral venous sinus thrombosisCerebral venous sinus thrombosisCerebral venous sinus thrombosis is a rare form of stroke that results from thrombosis of the dural venous sinuses, which drain blood from the brain. Symptoms may include headache, abnormal vision, any of the symptoms of stroke such as weakness of the face and limbs on one side of the body, and...
- Acute liver failure
- craniosynostosisCraniosynostosisCraniosynostosis is a condition in which one or more of the fibrous sutures in an infant skull prematurely fuses by ossification, thereby changing the growth pattern of the skull...
Signs and symptoms
In general, symptoms and signs that suggest a rise in ICP including headacheHeadache
A headache or cephalalgia is pain anywhere in the region of the head or neck. It can be a symptom of a number of different conditions of the head and neck. The brain tissue itself is not sensitive to pain because it lacks pain receptors. Rather, the pain is caused by disturbance of the...
, vomiting
Vomiting
Vomiting is the forceful expulsion of the contents of one's stomach through the mouth and sometimes the nose...
without nausea
Nausea
Nausea , is a sensation of unease and discomfort in the upper stomach with an involuntary urge to vomit. It often, but not always, precedes vomiting...
, ocular palsies, altered level of consciousness, back pain and papilledema
Papilledema
Papilledema is optic disc swelling that is caused by increased intracranial pressure. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare....
. If papilledema is protracted, it may lead to visual disturbances, optic atrophy, and eventually blindness.
In addition to the above, if mass effect is present with resulting displacement of brain tissue, additional signs may include pupillary dilatation, abducens palsies
Sixth nerve palsy
Sixth nerve palsy, or abducens nerve palsy, is a disorder associated with dysfunction of cranial nerve VI , which is responsible for contracting the lateral rectus muscle to abduct the eye...
, and the Cushing's triad
Cushing's triad
Cushing's triad is a clinical triad variably defined as either hypertension, bradycardia, andirregular respiration , or less commonly as widened pulse pressure , irregular respiration, and bradycardia...
. Cushing's triad involves an increased systolic blood pressure, a widened pulse pressure
Pulse pressure
Pulse Pressure is most easily defined as being the amount of pressure required to create the feeling of a pulse. Measured in millimeters of mercury , the pressure difference between the systolic and diastolic pressures give you the amount of pressure change to create the pulse, which is the pulse...
, bradycardia
Bradycardia
Bradycardia , in the context of adult medicine, is the resting heart rate of under 60 beats per minute, though it is seldom symptomatic until the rate drops below 50 beat/min. It may cause cardiac arrest in some patients, because those with bradycardia may not be pumping enough oxygen to their heart...
, and an abnormal respiratory pattern. In children, a slow heart rate is especially suggestive of high ICP.
Irregular respirations occur when injury to parts of the brain interfere with the respiratory drive. Cheyne-Stokes respiration
Cheyne-Stokes respiration
Cheyne-Stokes respiration is an abnormal pattern of breathing characterized by progressively deeper and sometimes faster breathing, followed by a gradual decrease that results in a temporary stop in breathing called an apnea. The pattern repeats, with each cycle usually taking 30 seconds to 2...
, in which breathing is rapid for a period and then absent for a period, occurs because of injury to the cerebral hemisphere
Cerebral hemisphere
A cerebral hemisphere is one of the two regions of the eutherian brain that are delineated by the median plane, . The brain can thus be described as being divided into left and right cerebral hemispheres. Each of these hemispheres has an outer layer of grey matter called the cerebral cortex that is...
s or diencephalon
Diencephalon
The diencephalon is the region of the vertebrate neural tube which gives rise to posterior forebrain structures. In development, the forebrain develops from the prosencephalon, the most anterior vesicle of the neural tube which later forms both the diencephalon and the...
. Hyperventilation
Hyperventilation
Hyperventilation or overbreathing is the state of breathing faster or deeper than normal, causing excessive expulsion of circulating carbon dioxide. It can result from a psychological state such as a panic attack, from a physiological condition such as metabolic acidosis, can be brought about by...
can occur when the brain stem
Brain stem
In vertebrate anatomy the brainstem is the posterior part of the brain, adjoining and structurally continuous with the spinal cord. The brain stem provides the main motor and sensory innervation to the face and neck via the cranial nerves...
or tegmentum
Tegmentum
The tegmentum is a general area within the brainstem. It is located between the ventricular system and distinctive basal or ventral structures at each level...
is damaged.
As a rule, patients with normal blood pressure retain normal alertness with ICP of 25–40 mmHg (unless tissue shifts at the same time). Only when ICP exceeds 40–50 mmHg do CPP and cerebral perfusion decrease to a level that results in loss of consciousness. Any further elevations will lead to brain infarction and brain death.
In infants and small children, the effects of ICP differ because their cranial sutures have not closed. In infants, the fontanels, or soft spots on the head where the skull bones have not yet fused, bulge when ICP gets too high.
A swollen optic nerve is a reliable sign that ICP is elevated.
Treatment
The treatment for IH depends on the etiologyEtiology
Etiology is the study of causation, or origination. The word is derived from the Greek , aitiologia, "giving a reason for" ....
. In addition to management of the underlying causes, major considerations in acute treatment of increased ICP relates to the management of stroke and cerebral trauma.
A very common treatment for long-term, especially idiopathic
Idiopathic
Idiopathic is an adjective used primarily in medicine meaning arising spontaneously or from an obscure or unknown cause. From Greek ἴδιος, idios + πάθος, pathos , it means approximately "a disease of its own kind". It is technically a term from nosology, the classification of disease...
, cranial hypertension is medication with a special diuretic
Diuretic
A diuretic provides a means of forced diuresis which elevates the rate of urination. There are several categories of diuretics. All diuretics increase the excretion of water from bodies, although each class does so in a distinct way.- Medical uses :...
, especially one prescribed by a neurologist
Neurologist
A neurologist is a physician who specializes in neurology, and is trained to investigate, or diagnose and treat neurological disorders.Neurology is the medical specialty related to the human nervous system. The nervous system encompasses the brain, spinal cord, and peripheral nerves. A specialist...
.
In patients who have high ICP due to an acute injury it is particularly important to ensure adequate airway
Airway
The pulmonary airway comprises those parts of the respiratory system through which air flows, conceptually beginning at the nose and mouth, and terminating in the alveoli...
, breathing, and oxygen
Oxygen
Oxygen is the element with atomic number 8 and represented by the symbol O. Its name derives from the Greek roots ὀξύς and -γενής , because at the time of naming, it was mistakenly thought that all acids required oxygen in their composition...
ation. Inadequate blood oxygen levels (hypoxia
Hypoxia (medical)
Hypoxia, or hypoxiation, is a pathological condition in which the body as a whole or a region of the body is deprived of adequate oxygen supply. Variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise...
) or excessively high carbon dioxide
Carbon dioxide
Carbon dioxide is a naturally occurring chemical compound composed of two oxygen atoms covalently bonded to a single carbon atom...
levels (hypercapnia
Hypercapnia
Hypercapnia or hypercapnea , also known as hypercarbia, is a condition where there is too much carbon dioxide in the blood...
) cause cerebral blood vessels to dilate, increasing the flow of blood to the brain and causing the ICP to rise. Inadequate oxygenation also forces brain cells to produce energy using anaerobic metabolism
Fermentation (biochemistry)
Fermentation is the process of extracting energy from the oxidation of organic compounds, such as carbohydrates, using an endogenous electron acceptor, which is usually an organic compound. In contrast, respiration is where electrons are donated to an exogenous electron acceptor, such as oxygen,...
, which produces lactic acid
Lactic acid
Lactic acid, also known as milk acid, is a chemical compound that plays a role in various biochemical processes and was first isolated in 1780 by the Swedish chemist Carl Wilhelm Scheele. Lactic acid is a carboxylic acid with the chemical formula C3H6O3...
and lowers pH
PH
In chemistry, pH is a measure of the acidity or basicity of an aqueous solution. Pure water is said to be neutral, with a pH close to 7.0 at . Solutions with a pH less than 7 are said to be acidic and solutions with a pH greater than 7 are basic or alkaline...
, also dilating blood vessels and exacerbating the problem. Conversely, blood vessels constrict when carbon dioxide levels are below normal, so hyperventilating a patient with a ventilator or bag valve mask
Bag valve mask
A bag valve mask is a hand-held device used to provide positive pressure ventilation to a patient who is not breathing or who is breathing inadequately. The device is a normal part of a resuscitation kit for trained professionals, such as ambulance crew...
can temporarily reduce ICP. Hyperventilation was formerly a part of the standard treatment of traumatic brain injuries, but the induced constriction of blood vessels limits blood flow to the brain at a time when the brain may already be ischemic -- hence it is no longer widely used. Furthermore, the brain adjusts to the new level of carbon dioxide after 48 to 72 hours of hyperventilation, which could cause the vessels to rapidly dilate if carbon-dioxide levels were returned to normal too quickly. Hyperventilation is still used if ICP is resistant to other methods of control, or there are signs of brain herniation
Brain herniation
Brain herniation, also known as cistern obliteration, is a deadly side effect of very high intracranial pressure that occurs when the brain shifts across structures within the skull...
because the damage herniation can cause is so severe that it may be worthwhile to constrict blood vessels even if doing so reduces blood flow. ICP can also be lowered by raising the head of the bed, improving venous drainage. A side effect of this is that it could lower pressure of blood to the head, resulting in a reduced and possibly inadequate blood supply to the brain. Venous drainage may also be impeded by external factors such as hard collars to immobilize the neck in trauma patients, and this may also increase the ICP. Sandbags may be used to further limit neck movement.
In the hospital, the blood pressure can be artificially increased in order to increase CPP, increase perfusion, oxygenate tissues, remove wastes and thereby lessen swelling. Since hypertension
Hypertension
Hypertension or high blood pressure is a cardiac chronic medical condition in which the systemic arterial blood pressure is elevated. What that means is that the heart is having to work harder than it should to pump the blood around the body. Blood pressure involves two measurements, systolic and...
is the body's way of forcing blood into the brain, medical professionals do not normally interfere with it when it is found in a patient with a head injury. When it is necessary to decrease cerebral blood flow, MAP can be lowered using common antihypertensive agents such as calcium channel blocker
Calcium channel blocker
A calcium channel blocker is a chemical that disrupts the movement of calcium through calcium channels.CCB drugs devised to target neurons are used as antiepileptics. However, the most widespread clinical usage of calcium channel blockers is to decrease blood pressure in patients with...
s. If there is an intact blood-brain barrier
Blood-brain barrier
The blood–brain barrier is a separation of circulating blood and the brain extracellular fluid in the central nervous system . It occurs along all capillaries and consists of tight junctions around the capillaries that do not exist in normal circulation. Endothelial cells restrict the diffusion...
, osmotherapy
Osmotherapy
Osmotherapy is a medical treatment, using intravenous injection or oral administration of an agent to induce dehydration. The goal of dehydration is to reduce the amount of accumulated fluid in the brain. The earliest description in medical literature dates back to 1919.- Treatment :Osmotherapy can...
may be carried out by administering IV
Intravenous therapy
Intravenous therapy or IV therapy is the infusion of liquid substances directly into a vein. The word intravenous simply means "within a vein". Therapies administered intravenously are often called specialty pharmaceuticals...
mannitol
Mannitol
Mannitol is a white, crystalline organic compound with the formula . This polyol is used as an osmotic diuretic agent and a weak renal vasodilator...
to create a hypertonic solution within the blood to draw water out of the neurons. This helps to reduce the fluid within the intracranial space, however prolonged administration may lead to increase in ICP.
Struggling, restlessness, and seizures can increase metabolic
Metabolism
Metabolism is the set of chemical reactions that happen in the cells of living organisms to sustain life. These processes allow organisms to grow and reproduce, maintain their structures, and respond to their environments. Metabolism is usually divided into two categories...
demands and oxygen consumption, as well as increasing blood pressure. Analgesia and sedation (particularly in the pre-hospital, ER, and intensive care setting) are used to reduce agitation and metabolic needs of the brain, but these medications may cause low blood pressure and other side effects. Thus if full sedation alone is ineffective, patients may be paralyzed
Paralysis
Paralysis is loss of muscle function for one or more muscles. Paralysis can be accompanied by a loss of feeling in the affected area if there is sensory damage as well as motor. A study conducted by the Christopher & Dana Reeve Foundation, suggests that about 1 in 50 people have been diagnosed...
with drugs such as atracurium
Atracurium
Atracurium besylate is a neuromuscular-blocking drug or skeletal muscle relaxant in the category of non-depolarizing neuromuscular-blocking drugs, used adjunctively in anesthesia to facilitate endotracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical...
. Paralysis allows the cerebral veins to drain more easily, but can mask signs of seizure
Seizure
An epileptic seizure, occasionally referred to as a fit, is defined as a transient symptom of "abnormal excessive or synchronous neuronal activity in the brain". The outward effect can be as dramatic as a wild thrashing movement or as mild as a brief loss of awareness...
s, and the drugs can have other harmful effects. Paralysing drugs are only introduced if patients are fully sedated (this is essentially the same as a general anaesthetic
General anaesthetic
A general anaesthetic is a drug that brings about a reversible loss of consciousness. These drugs are generally administered by an anaesthesia provider to induce or maintain general anaesthesia to facilitate surgery...
)
Intracranial pressure can be measured continuously with intracranial transducers. A catheter
Catheter
In medicine, a catheter is a tube that can be inserted into a body cavity, duct, or vessel. Catheters thereby allow drainage, administration of fluids or gases, or access by surgical instruments. The process of inserting a catheter is catheterization...
can be surgically inserted into one of the brain's lateral ventricle
Ventricular system
The ventricular system is a set of structures containing cerebrospinal fluid in the brain. It is continuous with the central canal of the spinal cord.-Components:The system comprises four ventricles:* right and left lateral ventricles* third ventricle...
s and can be used to drain CSF (cerebrospinal fluid) in order to decrease ICP's. This type of drain is known as an EVD (extraventricular drain
Extraventricular drain
An external ventricular drain , also known as a ventriculostomy, is a device used in neurosurgery that relieves raised intracranial pressure and hydrocephalus when the normal flow of cerebrospinal fluid around the brain is obstructed...
). In rare situations when only small amounts of CSF are to be drained to reduce ICP's, drainage of CSF via lumbar puncture can be used as a treatment. There are many clinical studies of non-invasive intracranial pressure measurement methods
Non-invasive intracranial pressure measurement methods
Increased intracranial pressure is one of the major causes of secondary brain ischemia that accompanies a variety of pathological conditions, most notably, traumatic brain injury , stroke, and intracranial hemorrhages...
currently being implemented, aimed to find reliable and accurate way to measure ICP non-invasively. Such method could improve diagnostics of traumatic brain injury and many other conditions associated with intracranial hypertension.
Craniotomies
Craniotomy
A craniotomy is a surgical operation in which a bone flap is temporarily removed from the skull to access the brain. Craniotomies are often a critical operation performed on patients recording, brain imaging, and for neurological manipulations such as electrical stimulation and chemical...
are holes drilled in the skull to remove intracranial hematomas or relieve pressure from parts of the brain. As raised ICP's may be caused by the presence of a mass, removal of this via craniotomy will decrease raised ICP's.
A drastic treatment for increased ICP is decompressive craniectomy
Decompressive craniectomy
Decompressive craniectomy is a neurosurgical procedure in which part of the skull is removed to allow a swelling brain room to expand without being squeezed. It is performed on victims of traumatic brain injury and stroke. Use of the surgery is controversial....
, in which a part of the skull is removed and the dura mater
Dura mater
The dura mater , or dura, is the outermost of the three layers of the meninges surrounding the brain and spinal cord. It is derived from Mesoderm. The other two meningeal layers are the pia mater and the arachnoid mater. The dura surrounds the brain and the spinal cord and is responsible for...
is expanded to allow the brain to swell without crushing it or causing herniation. The section of bone removed, known as a bone flap, can be stored in the patient's abdomen and resited back to complete the skull once the acute cause of raised ICP's has resolved. Alternatively a synthetic material may be used to replace the removed bone section (see cranioplasty
Cranioplasty
Cranioplasty is a surgical repair of a defect or deformity of a skull. Cranioplasty is almost as ancient as trepanation. There is evidence that Incan surgeons were performing cranioplasty using precious metals and gourds...
)
Low ICP
It is also possible for the intracranial pressure to drop below normal levels, though increased intracranial pressure is a far more common (and far more serious) sign. The symptoms for both conditions are often the same, leading many medical experts to believe that it is the change in pressure rather than the pressure itself causing the above symptoms.Spontaneous intracranial hypotension may occur as a result of an occult leak of CSF into another body cavity. More commonly, decreased ICP is the result of lumbar puncture or other medical procedures involving the brain or spinal cord. Various medical imaging technologies exist to assist in identifying the cause of decreased ICP. Often, the syndrome is self-limiting, especially if it is the result of a medical procedure. If persistent intracranial hypotension is the result of a lumbar puncture, a "blood patch" may be applied to seal the site of CSF leakage. Various medical treatments have been proposed; only the intravenous administration of caffeine
Caffeine
Caffeine is a bitter, white crystalline xanthine alkaloid that acts as a stimulant drug. Caffeine is found in varying quantities in the seeds, leaves, and fruit of some plants, where it acts as a natural pesticide that paralyzes and kills certain insects feeding on the plants...
and theophylline
Theophylline
Theophylline, also known as dimethylxanthine, is a methylxanthine drug used in therapy for respiratory diseases such as COPD and asthma under a variety of brand names. Because of its numerous side-effects, the drug is now rarely administered for clinical use. As a member of the xanthine family, it...
has shown to be particularly useful.
External links
- Gruen P. 2002. "Monro-Kellie Model" Neurosurgery Infonet. USC Neurosurgery. Accessed January 4, 2007.
- National Guideline Clearinghouse. 2005. Guidelines for the management of severe traumatic brain injury. Firstgov. Accessed January 4, 2007.

