
Gestational diabetes
Encyclopedia
Gestational diabetes is a condition in which women without previously diagnosed diabetes
exhibit high blood glucose
levels during pregnancy
(especially during third trimester of pregnancy). It is widely accepted as a disease only in the United States, there is some question whether the condition is natural during pregnancy . Gestational diabetes is caused when the body of a pregnant woman does not secrete excess insulin required during pregnancy leading to increased blood sugar levels.
Gestational diabetes generally has few symptoms and it is most commonly diagnosed by screening
during pregnancy. Diagnostic tests detect inappropriately high levels of glucose
in blood samples. Gestational diabetes affects 3-10% of pregnancies, depending on the population studied, so may be a natural phenomenon.
As with diabetes mellitus in pregnancy in general, babies born to mothers with gestational diabetes are typically at increased risk of problems such as being large for gestational age (which may lead to delivery complications), low blood sugar
, and jaundice
. Gestational diabetes is a treatable condition and women who have adequate control of glucose levels can effectively decrease these risks.
Women with gestational diabetes are at increased risk of developing type 2 diabetes mellitus (or, very rarely, latent autoimmune diabetes
or Type 1
) after pregnancy, as well as having a higher incidence of pre-eclampsia
and Caesarean section
; their offspring are prone to developing childhood obesity
, with type 2 diabetes later in life. Most patients are treated only with diet modification and moderate exercise but some take anti-diabetic drugs, including insulin
.
Women treated for gestational diabetes, generally have smaller birthweight babies, leading to other problems, such as survival rate of premature and early births, particularly male babies.
The White classification, named after Priscilla White
who pioneered in research on the effect of diabetes types on perinatal outcome, is widely used to assess maternal and fetal risk. It distinguishes between gestational diabetes (type A) and diabetes that existed prior to pregnancy (pregestational diabetes). These two groups are further subdivided according to their associated risks and management.
There are 2 subtypes of gestational diabetes (diabetes which began during pregnancy):
The second group of diabetes which existed prior to pregnancy
is also split up into several subtypes.
In addition to this, statistics show a double risk of GDM in smokers
. Polycystic ovarian syndrome is also a risk factor, although relevant evidence remains controversial. Some studies have looked at more controversial potential risk factors, such as short stature
.
About 40-60% of women with GDM have no demonstrable risk factor; for this reason many advocate to screen all women. Typically women with gestational diabetes exhibit no symptoms (another reason for universal screening), but some women may demonstrate increased thirst
, increased urination
, fatigue, nausea
and vomiting
, bladder infection
, yeast infections and blurred vision
.
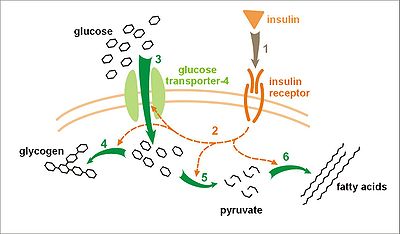 The precise mechanisms underlying gestational diabetes remain unknown. The hallmark of GDM is increased insulin resistance
The precise mechanisms underlying gestational diabetes remain unknown. The hallmark of GDM is increased insulin resistance
. Pregnancy hormones and other factors are thought to interfere with the action of insulin as it binds to the insulin receptor
. The interference probably occurs at the level of the cell signaling
pathway behind the insulin receptor. Since insulin promotes the entry of glucose into most cells, insulin resistance prevents glucose from entering the cells properly. As a result, glucose remains in the bloodstream, where glucose levels rise. More insulin is needed to overcome this resistance; about 1.5-2.5 times more insulin is produced than in a normal pregnancy.
Insulin resistance is a normal phenomenon emerging in the second trimester of pregnancy, which progresses thereafter to levels seen in non-pregnant patients with type 2 diabetes. It is thought to secure glucose supply to the growing fetus. Women with GDM have an insulin resistance they cannot compensate with increased production in the β-cells of the pancreas. Placenta
l hormones, and to a lesser extent increased fat
deposits during pregnancy, seem to mediate insulin resistance during pregnancy. Cortisol
and progesterone
are the main culprits, but human placental lactogen
, prolactin
and estradiol
contribute too.
It is unclear why some patients are unable to balance insulin needs and develop GDM, however a number of explanations have been given, similar to those in type 2 diabetes: autoimmunity
, single gene mutations, obesity, and other mechanisms.
Because glucose travels across the placenta (through diffusion facilitated
by GLUT3
carriers), the fetus is exposed to higher glucose levels. This leads to increased fetal levels of insulin
(insulin itself cannot cross the placenta). The growth-stimulating effects of insulin can lead to excessive growth and a large body (macrosomia). After birth, the high glucose environment disappears, leaving these newborns with ongoing high insulin production and susceptibility to low blood glucose levels (hypoglycemia
).
in plasma
or serum
in defined circumstances. One method is a stepwise approach where a suspicious result on a screening test is followed by diagnostic test. Alternatively, a more involved diagnostic test can be used directly at the first antenatal visit in high-risk patients (for example in those with polycystic ovarian syndrome or acanthosis nigricans
).
Non-challenge blood glucose tests involve measuring glucose levels in blood samples without challenging the subject with glucose solutions. A blood glucose level is determined when fasting, 2 hours after a meal, or simply at any random time. In contrast, challenge tests involve drinking a glucose solution and measuring glucose concentration thereafter in the blood; in diabetes, they tend to remain high. The glucose solution has a very sweet taste which some women find unpleasant; sometimes, therefore, artificial flavours are added. Some women may experience nausea during the test, and more so with higher glucose levels.
In the United States
, most obstetricians prefer universal screening with a screening glucose challenge test. In the United Kingdom
, obstetric units often rely on risk factors and a random blood glucose test. The American Diabetes Association
and the Society of Obstetricians and Gynaecologists of Canada
recommend routine screening unless the patient is low risk (this means the woman must be younger than 25 years and have a body mass index
less than 27, with no personal, ethnic or family risk factors) The Canadian Diabetes Association
and the American College of Obstetricians and Gynecologists recommend universal screening. The U.S. Preventive Services Task Force
found that there is insufficient evidence to recommend for or against routine screening.
If the cut-off point is set at 140 mg/dl (7.8 mmol/l), 80% of women with GDM will be detected. If this threshold for further testing is lowered to 130 mg/dl, 90% of GDM cases will be detected, but there will also be more women who will be subjected to a consequent OGTT unnecessarily.
per day) and unlimited physical activity. The subject should remain seated during the test and should not smoke throughout the test.
The test involves drinking a solution containing a certain amount of glucose, and drawing blood to measure glucose levels at the start and on set time intervals thereafter.
The diagnostic criteria from the National Diabetes Data Group (NDDG) have been used most often, but some centers rely on the Carpenter and Coustan criteria, which set the cutoff for normal at lower values. Compared with the NDDG criteria, the Carpenter and Coustan criteria lead to a diagnosis of gestational diabetes in 54 percent more pregnant women, with an increased cost and no compelling evidence of improved perinatal outcomes.
The following are the values which the American Diabetes Association
considers to be abnormal during the 100 g of glucose OGTT:
An alternative test uses a 75 g glucose load and measures the blood glucose levels before and after 1 and 2 hours, using the same reference values. This test will identify fewer women who are at risk, and there is only a weak concordance (agreement rate) between this test and a 3 hour 100 g test.
The glucose values used to detect gestational diabetes were first determined by O'Sullivan and Mahan (1964) in a retrospective cohort study
(using a 100 grams of glucose OGTT) designed to detect risk of developing type 2 diabetes in the future. The values were set using whole blood and required two values reaching or exceeding the value to be positive. Subsequent information led to alterations in O'Sullivan's criteria. When methods for blood glucose determination changed from the use of whole blood to venous plasma samples, the criteria for GDM were also changed.
testing is widely practiced, it performs poorly, and discontinuing routine dipstick testing has not been shown to cause underdiagnosis where universal screening is performed. Increased glomerular filtration rates during pregnancy contribute to some 50% of women having glucose in their urine on dipstick tests at some point during their pregnancy. The sensitivity of glucosuria for GDM in the first 2 trimesters is only around 10% and the positive predictive value
is around 20%.
 The goal of treatment is to reduce the risks of GDM for mother and child. Scientific evidence is beginning to show that controlling glucose levels can result in less serious fetal complications (such as macrosomia) and increased maternal quality of life
The goal of treatment is to reduce the risks of GDM for mother and child. Scientific evidence is beginning to show that controlling glucose levels can result in less serious fetal complications (such as macrosomia) and increased maternal quality of life
. Unfortunately, treatment of GDM is also accompanied by more infants admitted to neonatal wards and more inductions of labour, with no proven decrease in cesarean section rates or perinatal mortality
. These findings are still recent and controversial.
A repeat OGTT should be carried out 2–4 months after delivery, to confirm the diabetes has disappeared. Afterwards, regular screening for type 2 diabetes is advised.
If a diabetic diet
or G.I. Diet
, exercise, and oral medication are inadequate to control glucose levels, insulin therapy may become necessary.
The development of macrosomia can be evaluated during pregnancy by using sonography
. Women who use insulin, with a history of stillbirth, or with hypertension are managed like women with overt diabetes.
supplements) and multidisciplinary management are important for good pregnancy outcomes. Most women can manage their GDM with dietary changes and exercise. Self monitoring of blood glucose levels can guide therapy. Some women will need antidiabetic drugs, most commonly insulin
therapy.
Any diet needs to provide sufficient calories for pregnancy, typically 2,000 - 2,500 kcal with the exclusion of simple carbohydrates. The main goal of dietary modifications is to avoid peaks in blood sugar levels. This can be done by spreading carbohydrate intake over meals and snacks throughout the day, and using slow-release carbohydrate sources—known as the G.I. Diet
. Since insulin resistance is highest in mornings, breakfast carbohydrates need to be restricted more. Ingesting more fiber in foods with whole grains, or fruit and vegetables can also reduce the risk of gestational diabetes.
Regular moderately intense physical exercise is advised, although there is no consensus on the specific structure of exercise programs for GDM.
Self monitoring can be accomplished using a handheld capillary glucose dosage system. Compliance with these glucometer systems can be low. Target ranges advised by the Australasian Diabetes in Pregnancy Society are as follows:
Regular blood samples can be used to determine HbA1c levels, which give an idea of glucose control over a longer time period.
Research suggests a possible benefit of breastfeeding
to reduce the risk of diabetes and related risks for both mother and child.
) due to excessive insulin injections. Insulin therapy can be normal or very tight; more injections can result in better control but requires more effort, and there is no consensus that it has large benefits.
There is some evidence that certain oral glycemic agents might be safe in pregnancy, or at least, are significantly less dangerous to the developing fetus than poorly controlled diabetes. Glyburide, a second generation sulfonylurea
, has been shown to be an effective alternative to insulin therapy. In one study, 4% of women needed supplemental insulin to reach blood sugar targets.
Metformin
has shown promising results, with its oral format being much more popular than insulin injections. Treatment of polycystic ovarian syndrome with metformin during pregnancy has been noted to decrease GDM levels. A recent randomized controlled trial
of metformin versus insulin showed that women preferred metformin tablets to insulin injections, and that metformin is safe and equally effective as insulin. Severe neonatal hypoglycemia was less common in insulin-treated women, but preterm delivery was more common. Almost half of patients did not reach sufficient control with metformin alone and needed supplemental therapy with insulin; compared to those treated with insulin alone, they required less insulin, and they gained less weight. With no long-term studies into children of women treated with the drug, here remains a possibility of long-term complications from metformin therapy, although follow-up at the age of 18 months of children born to women with polycystic ovarian syndrome and treated with metformin revealed no developmental abnormalities.
Women diagnosed with gestational diabetes have an increased risk of developing diabetes mellitus in the future. The risk is highest in women who needed insulin treatment, had antibodies
associated with diabetes (such as antibodies against glutamate decarboxylase
, islet cell antibodies and/or insulinoma antigen-2), women with more than two previous pregnancies, and women who were obese (in order of importance). Women requiring insulin to manage gestational diabetes have a 50% risk of developing diabetes within the next five years. Depending on the population studied, the diagnostic criteria and the length of follow-up, the risk can vary enormously. The risk appears to be highest in the first 5 years, reaching a plateau thereafter. One of the longest studies followed a group of women from Boston, Massachusetts; half of them developed diabetes after 6 years, and more than 70% had diabetes after 28 years. In a retrospective study in Navajo
women, the risk of diabetes after GDM was estimated to be 50 to 70% after 11 years. Another study found a risk of diabetes after GDM of more than 25% after 15 years. In populations with a low risk for type 2 diabetes, in lean subjects and in patients with auto-antibodies
, there is a higher rate of women developing type 1 diabetes.
Children of women with GDM have an increased risk for childhood and adult obesity and an increased risk of glucose intolerance and type 2 diabetes later in life. This risk relates to increased maternal glucose values. It is currently unclear how much genetic susceptibility and environmental factors each contribute to this risk, and if treatment of GDM can influence this outcome.
There are scarce statistical data on the risk of other conditions in women with GDM; in the Jerusalem Perinatal study, 410 out of 37962 patients were reported to have GDM, and there was a tendency towards more breast and pancreatic cancer, but more research is needed to confirm this finding.
The two main risks GDM imposes on the baby are growth abnormalities and chemical imbalances after birth, which may require admission to a neonatal intensive care unit
. Infants born to mothers with GDM are at risk of being both large for gestational age
(macrosomic) and small for gestational age
. Macrosomia in turn increases the risk of instrumental deliveries (e.g. forceps
, ventouse
and caesarean section
) or problems during vaginal delivery (such as shoulder dystocia
). Macrosomia may affect 12% of normal women compared to 20% of patients with GDM. However, the evidence for each of these complications is not equally strong; in the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study for example, there was an increased risk for babies to be large but not small for gestational age. Research into complications for GDM is difficult because of the many confounding factors (such as obesity). Labelling a woman as having GDM may in itself increase the risk of having a caesarean section.
Neonates are also at an increased risk of low blood glucose (hypoglycemia
), jaundice
, high red blood cell
mass (polycythemia
) and low blood calcium (hypocalcemia) and magnesium (hypomagnesemia
). GDM also interferes with maturation, causing dysmature babies prone to respiratory distress syndrome
due to incomplete lung maturation and impaired surfactant
synthesis.
Unlike pre-gestational diabetes, gestational diabetes has not been clearly shown to be an independent risk factor for birth defects. Birth defects usually originate sometime during the first trimester (before the 13th week) of pregnancy, whereas GDM gradually develops and is least pronounced during the first trimester. Studies have shown that the offspring of women with GDM are at a higher risk for congenital malformations. A large case-control study found that gestational diabetes was linked with a limited group of birth defects, and that this association was generally limited to women with a higher body mass index (≥ 25 kg/m²). It is difficult to make sure that this is not partially due to the inclusion of women with pre-existent type 2 diabetes who were not diagnosed before pregnancy.
Because of conflicting studies, it is unclear at the moment whether women with GDM have a higher risk of preeclampsia. In the HAPO study, the risk of preeclampsia was between 13% and 37% higher, although not all possible confounding factors were corrected.
Diabetes mellitus
Diabetes mellitus, often simply referred to as diabetes, is a group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin, or because cells do not respond to the insulin that is produced...
exhibit high blood glucose
Hyperglycemia
Hyperglycemia or Hyperglycæmia, or high blood sugar, is a condition in which an excessive amount of glucose circulates in the blood plasma. This is generally a glucose level higher than 13.5mmol/l , but symptoms may not start to become noticeable until even higher values such as 15-20 mmol/l...
levels during pregnancy
Pregnancy
Pregnancy refers to the fertilization and development of one or more offspring, known as a fetus or embryo, in a woman's uterus. In a pregnancy, there can be multiple gestations, as in the case of twins or triplets...
(especially during third trimester of pregnancy). It is widely accepted as a disease only in the United States, there is some question whether the condition is natural during pregnancy . Gestational diabetes is caused when the body of a pregnant woman does not secrete excess insulin required during pregnancy leading to increased blood sugar levels.
Gestational diabetes generally has few symptoms and it is most commonly diagnosed by screening
Screening (medicine)
Screening, in medicine, is a strategy used in a population to detect a disease in individuals without signs or symptoms of that disease. Unlike what generally happens in medicine, screening tests are performed on persons without any clinical sign of disease....
during pregnancy. Diagnostic tests detect inappropriately high levels of glucose
Glucose
Glucose is a simple sugar and an important carbohydrate in biology. Cells use it as the primary source of energy and a metabolic intermediate...
in blood samples. Gestational diabetes affects 3-10% of pregnancies, depending on the population studied, so may be a natural phenomenon.
As with diabetes mellitus in pregnancy in general, babies born to mothers with gestational diabetes are typically at increased risk of problems such as being large for gestational age (which may lead to delivery complications), low blood sugar
Hypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
, and jaundice
Jaundice
Jaundice is a yellowish pigmentation of the skin, the conjunctival membranes over the sclerae , and other mucous membranes caused by hyperbilirubinemia . This hyperbilirubinemia subsequently causes increased levels of bilirubin in the extracellular fluid...
. Gestational diabetes is a treatable condition and women who have adequate control of glucose levels can effectively decrease these risks.
Women with gestational diabetes are at increased risk of developing type 2 diabetes mellitus (or, very rarely, latent autoimmune diabetes
Latent autoimmune diabetes
Latent Autoimmune Diabetes of Adults , also known as, Diabetes Type 1.5, is a term coined by Tuomi et al. in 1993 to describe slow-onset Type 1 autoimmune diabetes in adults...
or Type 1
Diabetes mellitus type 1
Diabetes mellitus type 1 is a form of diabetes mellitus that results from autoimmune destruction of insulin-producing beta cells of the pancreas. The subsequent lack of insulin leads to increased blood and urine glucose...
) after pregnancy, as well as having a higher incidence of pre-eclampsia
Pre-eclampsia
Pre-eclampsia or preeclampsia is a medical condition in which hypertension arises in pregnancy in association with significant amounts of protein in the urine....
and Caesarean section
Caesarean section
A Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
; their offspring are prone to developing childhood obesity
Childhood obesity
Childhood obesity is a condition where excess body fat negatively affects a child's health or wellbeing. As methods to determine body fat directly are difficult, the diagnosis of obesity is often based on BMI. Due to the rising prevalence of obesity in children and its many adverse health effects...
, with type 2 diabetes later in life. Most patients are treated only with diet modification and moderate exercise but some take anti-diabetic drugs, including insulin
Insulin
Insulin is a hormone central to regulating carbohydrate and fat metabolism in the body. Insulin causes cells in the liver, muscle, and fat tissue to take up glucose from the blood, storing it as glycogen in the liver and muscle....
.
Women treated for gestational diabetes, generally have smaller birthweight babies, leading to other problems, such as survival rate of premature and early births, particularly male babies.
Classification
Gestational diabetes is formally defined as "any degree of glucose intolerance with onset or first recognition during pregnancy". This definition acknowledges the possibility that patients may have previously undiagnosed diabetes mellitus, or may have developed diabetes coincidentally with pregnancy. Whether symptoms subside after pregnancy is also irrelevant to the diagnosis.The White classification, named after Priscilla White
Priscilla White (physician)
Priscilla White, M.D. was a pioneer in the treatment of diabetes during pregnancy and type 1 diabetes, and was also a founding member of the Joslin Diabetes Center....
who pioneered in research on the effect of diabetes types on perinatal outcome, is widely used to assess maternal and fetal risk. It distinguishes between gestational diabetes (type A) and diabetes that existed prior to pregnancy (pregestational diabetes). These two groups are further subdivided according to their associated risks and management.
There are 2 subtypes of gestational diabetes (diabetes which began during pregnancy):
- Type A1: abnormal oral glucose tolerance test (OGTT) but normal blood glucose levels during fasting and 2 hours after meals; diet modification is sufficient to control glucose levels
- Type A2: abnormal OGTT compounded by abnormal glucose levels during fasting and/or after meals; additional therapy with insulin or other medications is required
The second group of diabetes which existed prior to pregnancy
Diabetes mellitus and pregnancy
For women with diabetes mellitus, pregnancy can present some particular challenges for both mother and child. If the woman who is pregnant has diabetes, it can cause early labor, birth defects, and very large babies....
is also split up into several subtypes.
Risk Factors
Classical risk factors for developing gestational diabetes are the following:- a previous diagnosis of gestational diabetes or prediabetes, impaired glucose toleranceImpaired glucose toleranceImpaired glucose tolerance is a pre-diabetic state of dysglycemia that is associated with insulin resistance and increased risk of cardiovascular pathology. IGT may precede type 2 diabetes mellitus by many years...
, or impaired fasting glycaemiaImpaired fasting glycaemiaImpaired fasting glucose , more commonly known as pre-diabetes refers to a condition in which the fasting blood glucose level is consistently elevated above what is considered normal levels; however, it is not high enough to be diagnosed as diabetes mellitus... - a family historyFamily history (medicine)In medicine, a family history consists of information about disorders from which the direct blood relatives of the patient have suffered. Genealogy typically includes very little of the medical history of the family, but the medical history could be considered a specific subset of the total history...
revealing a first degree relative with type 2 diabetesDiabetes mellitus type 2Diabetes mellitus type 2formerly non-insulin-dependent diabetes mellitus or adult-onset diabetesis a metabolic disorder that is characterized by high blood glucose in the context of insulin resistance and relative insulin deficiency. Diabetes is often initially managed by increasing exercise and... - maternal age - a woman's risk factor increases as she gets older (especially for women over 35 years of age)
- ethnic background (those with higher risk factors include African-Americans, Afro-Caribbeans, Native AmericansIndigenous peoples of the AmericasThe indigenous peoples of the Americas are the pre-Columbian inhabitants of North and South America, their descendants and other ethnic groups who are identified with those peoples. Indigenous peoples are known in Canada as Aboriginal peoples, and in the United States as Native Americans...
, Hispanics, Pacific Islanders, and people originating from South AsiaSouth AsiaSouth Asia, also known as Southern Asia, is the southern region of the Asian continent, which comprises the sub-Himalayan countries and, for some authorities , also includes the adjoining countries to the west and the east...
) - being overweightOverweightOverweight is generally defined as having more body fat than is optimally healthy. Being overweight is a common condition, especially where food supplies are plentiful and lifestyles are sedentary...
, obeseObesityObesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health, leading to reduced life expectancy and/or increased health problems...
or severely obese increases the risk by a factor 2.1, 3.6 and 8.6, respectively. - a previous pregnancy which resulted in a child with a high birth weight (>90th centile, or >4000 g (8 lbs 12.8 oz))
- previous poor obstetric history
In addition to this, statistics show a double risk of GDM in smokers
Smoking
Smoking is a practice in which a substance, most commonly tobacco or cannabis, is burned and the smoke is tasted or inhaled. This is primarily practised as a route of administration for recreational drug use, as combustion releases the active substances in drugs such as nicotine and makes them...
. Polycystic ovarian syndrome is also a risk factor, although relevant evidence remains controversial. Some studies have looked at more controversial potential risk factors, such as short stature
Short stature
Short stature refers to a height of a human being which is below expected. Shortness is a vague term without a precise definition and with significant relativity to context...
.
About 40-60% of women with GDM have no demonstrable risk factor; for this reason many advocate to screen all women. Typically women with gestational diabetes exhibit no symptoms (another reason for universal screening), but some women may demonstrate increased thirst
Thirst
Thirst is the craving for fluids, resulting in the basic instinct of animals to drink. It is an essential mechanism involved in fluid balance. It arises from a lack of fluids and/or an increase in the concentration of certain osmolites, such as salt...
, increased urination
Urination
Urination, also known as micturition, voiding, peeing, weeing, pissing, and more rarely, emiction, is the ejection of urine from the urinary bladder through the urethra to the outside of the body. In healthy humans the process of urination is under voluntary control...
, fatigue, nausea
Nausea
Nausea , is a sensation of unease and discomfort in the upper stomach with an involuntary urge to vomit. It often, but not always, precedes vomiting...
and vomiting
Vomiting
Vomiting is the forceful expulsion of the contents of one's stomach through the mouth and sometimes the nose...
, bladder infection
Cystitis
Cystitis is a term that refers to urinary bladder inflammation that results from any one of a number of distinct syndromes. It is most commonly caused by a bacterial infection in which case it is referred to as a urinary tract infection.-Signs and symptoms:...
, yeast infections and blurred vision
Blurred vision
-Causes:There are many causes of blurred vision:* Use of atropine or other anticholinergics* Presbyopia -- Difficulty focusing on objects that are close. The elderly are common victims....
.
Pathophysiology
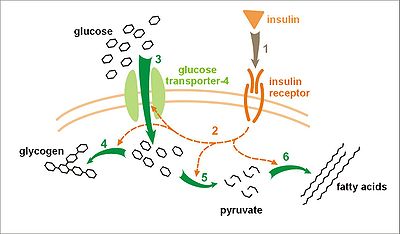
Insulin resistance
Insulin resistance is a physiological condition where the natural hormone insulin becomes less effective at lowering blood sugars. The resulting increase in blood glucose may raise levels outside the normal range and cause adverse health effects, depending on dietary conditions. Certain cell types...
. Pregnancy hormones and other factors are thought to interfere with the action of insulin as it binds to the insulin receptor
Insulin receptor
In molecular biology, the insulin receptor is a transmembrane receptor that is activated by insulin. It belongs to the large class of tyrosine kinase receptors....
. The interference probably occurs at the level of the cell signaling
Cell signaling
Cell signaling is part of a complex system of communication that governs basic cellular activities and coordinates cell actions. The ability of cells to perceive and correctly respond to their microenvironment is the basis of development, tissue repair, and immunity as well as normal tissue...
pathway behind the insulin receptor. Since insulin promotes the entry of glucose into most cells, insulin resistance prevents glucose from entering the cells properly. As a result, glucose remains in the bloodstream, where glucose levels rise. More insulin is needed to overcome this resistance; about 1.5-2.5 times more insulin is produced than in a normal pregnancy.
Insulin resistance is a normal phenomenon emerging in the second trimester of pregnancy, which progresses thereafter to levels seen in non-pregnant patients with type 2 diabetes. It is thought to secure glucose supply to the growing fetus. Women with GDM have an insulin resistance they cannot compensate with increased production in the β-cells of the pancreas. Placenta
Placenta
The placenta is an organ that connects the developing fetus to the uterine wall to allow nutrient uptake, waste elimination, and gas exchange via the mother's blood supply. "True" placentas are a defining characteristic of eutherian or "placental" mammals, but are also found in some snakes and...
l hormones, and to a lesser extent increased fat
Fat
Fats consist of a wide group of compounds that are generally soluble in organic solvents and generally insoluble in water. Chemically, fats are triglycerides, triesters of glycerol and any of several fatty acids. Fats may be either solid or liquid at room temperature, depending on their structure...
deposits during pregnancy, seem to mediate insulin resistance during pregnancy. Cortisol
Cortisol
Cortisol is a steroid hormone, more specifically a glucocorticoid, produced by the adrenal gland. It is released in response to stress and a low level of blood glucocorticoids. Its primary functions are to increase blood sugar through gluconeogenesis; suppress the immune system; and aid in fat,...
and progesterone
Progesterone
Progesterone also known as P4 is a C-21 steroid hormone involved in the female menstrual cycle, pregnancy and embryogenesis of humans and other species...
are the main culprits, but human placental lactogen
Human placental lactogen
Human placental lactogen , also called human chorionic somatomammotropin, is a polypeptide placental hormone. Its structure and function is similar to that of human growth hormone. It modifies the metabolic state of the mother during pregnancy to facilitate the energy supply of the fetus. HPL has...
, prolactin
Prolactin
Prolactin also known as luteotropic hormone is a protein that in humans is encoded by the PRL gene.Prolactin is a peptide hormone discovered by Henry Friesen...
and estradiol
Estradiol
Estradiol is a sex hormone. Estradiol is abbreviated E2 as it has 2 hydroxyl groups in its molecular structure. Estrone has 1 and estriol has 3 . Estradiol is about 10 times as potent as estrone and about 80 times as potent as estriol in its estrogenic effect...
contribute too.
It is unclear why some patients are unable to balance insulin needs and develop GDM, however a number of explanations have been given, similar to those in type 2 diabetes: autoimmunity
Autoimmunity
Autoimmunity is the failure of an organism to recognize its own constituent parts as self, which allows an immune response against its own cells and tissues. Any disease that results from such an aberrant immune response is termed an autoimmune disease...
, single gene mutations, obesity, and other mechanisms.
Because glucose travels across the placenta (through diffusion facilitated
Facilitated diffusion
..Facilitated diffusion is a process of passive transport, facilitated by integral proteins. Facilitated diffusion is the spontaneous passage of molecules or ions across a biological membrane passing through specific transmembrane integral proteins...
by GLUT3
GLUT3
Glucose transporter 3 , also known as solute carrier family 2, facilitated glucose transporter member 3 is a protein that in humans is encoded by the SLC2A3 gene. GLUT3 facilitates the transport of glucose across the plasma membranes of mammalian cells...
carriers), the fetus is exposed to higher glucose levels. This leads to increased fetal levels of insulin
Insulin
Insulin is a hormone central to regulating carbohydrate and fat metabolism in the body. Insulin causes cells in the liver, muscle, and fat tissue to take up glucose from the blood, storing it as glycogen in the liver and muscle....
(insulin itself cannot cross the placenta). The growth-stimulating effects of insulin can lead to excessive growth and a large body (macrosomia). After birth, the high glucose environment disappears, leaving these newborns with ongoing high insulin production and susceptibility to low blood glucose levels (hypoglycemia
Hypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
).
Screening
A number of screening and diagnostic tests have been used to look for high levels of glucoseGlucose
Glucose is a simple sugar and an important carbohydrate in biology. Cells use it as the primary source of energy and a metabolic intermediate...
in plasma
Blood plasma
Blood plasma is the straw-colored liquid component of blood in which the blood cells in whole blood are normally suspended. It makes up about 55% of the total blood volume. It is the intravascular fluid part of extracellular fluid...
or serum
Blood serum
In blood, the serum is the component that is neither a blood cell nor a clotting factor; it is the blood plasma with the fibrinogens removed...
in defined circumstances. One method is a stepwise approach where a suspicious result on a screening test is followed by diagnostic test. Alternatively, a more involved diagnostic test can be used directly at the first antenatal visit in high-risk patients (for example in those with polycystic ovarian syndrome or acanthosis nigricans
Acanthosis nigricans
Acanthosis nigricans is a brown to black, poorly defined, velvety hyperpigmentation of the skin. It is usually found in body folds, such as the posterior and lateral folds of the neck, the axilla, groin, umbilicus, forehead, and other areas.-Causes:...
).
Non-challenge blood glucose test
|
| Screening glucose challenge test |
| Oral glucose tolerance test (OGTT) |
Non-challenge blood glucose tests involve measuring glucose levels in blood samples without challenging the subject with glucose solutions. A blood glucose level is determined when fasting, 2 hours after a meal, or simply at any random time. In contrast, challenge tests involve drinking a glucose solution and measuring glucose concentration thereafter in the blood; in diabetes, they tend to remain high. The glucose solution has a very sweet taste which some women find unpleasant; sometimes, therefore, artificial flavours are added. Some women may experience nausea during the test, and more so with higher glucose levels.
Pathways
There are different opinions about optimal screening and diagnostic measures, in part due to differences in population risks, cost-effectiveness considerations, and lack of an evidence base to support large national screening programs. The most elaborate regime entails a random blood glucose test during a booking visit, a screening glucose challenge test around 24–28 weeks' gestation, followed by an OGTT if the tests are outside normal limits. If there is a high suspicion, women may be tested earlier.In the United States
United States
The United States of America is a federal constitutional republic comprising fifty states and a federal district...
, most obstetricians prefer universal screening with a screening glucose challenge test. In the United Kingdom
United Kingdom
The United Kingdom of Great Britain and Northern IrelandIn the United Kingdom and Dependencies, other languages have been officially recognised as legitimate autochthonous languages under the European Charter for Regional or Minority Languages...
, obstetric units often rely on risk factors and a random blood glucose test. The American Diabetes Association
American Diabetes Association
The American Diabetes Association is a United States-based association working to fight the consequences of diabetes, and to help those affected by diabetes...
and the Society of Obstetricians and Gynaecologists of Canada
Society of Obstetricians and Gynaecologists of Canada
The Society of Obstetricians and Gynaecologists of Canada is a national medical society in Canada, representing over 3,000 obstetricians/gynecologists, family physicians, nurses, midwives, and allied health professionals in the field of sexual reproductive health...
recommend routine screening unless the patient is low risk (this means the woman must be younger than 25 years and have a body mass index
Body mass index
The body mass index , or Quetelet index, is a heuristic proxy for human body fat based on an individual's weight and height. BMI does not actually measure the percentage of body fat. It was invented between 1830 and 1850 by the Belgian polymath Adolphe Quetelet during the course of developing...
less than 27, with no personal, ethnic or family risk factors) The Canadian Diabetes Association
Canadian Diabetes Association
The Canadian Diabetes Association is an organization based in Toronto, Ontario, Canada. Its mission is to lead the fight against diabetes mellitus by helping Canadians with diabetes live healthy lives while work is continued to find a cure...
and the American College of Obstetricians and Gynecologists recommend universal screening. The U.S. Preventive Services Task Force
U.S. Preventive Services Task Force
The U.S. Preventive Services Task Force is "an independent panel of experts in primary care and prevention that systematically reviews the evidence of effectiveness and develops recommendations for clinical preventive services." The task force, a panel of primary care physicians and...
found that there is insufficient evidence to recommend for or against routine screening.
Non-challenge blood glucose tests
When a plasma glucose level is found to be higher than 126 mg/dl (7.0 mmol/l) after fasting, or over 200 mg/dl (11.1 mmol/l) on any occasion, and if this is confirmed on a subsequent day, the diagnosis of GDM is made, and no further testing is required. These tests are typically performed at the first antenatal visit. They are patient-friendly and inexpensive, but have a lower test performance compared to the other tests, with moderate sensitivity, low specificity and high false positive rates.Screening glucose challenge test
The screening glucose challenge test (sometimes called the O'Sullivan test) is performed between 24–28 weeks, and can be seen as a simplified version of the oral glucose tolerance test (OGTT). It involves drinking a solution containing 50 grams of glucose, and measuring blood levels 1 hour later.If the cut-off point is set at 140 mg/dl (7.8 mmol/l), 80% of women with GDM will be detected. If this threshold for further testing is lowered to 130 mg/dl, 90% of GDM cases will be detected, but there will also be more women who will be subjected to a consequent OGTT unnecessarily.
Oral glucose tolerance test
The OGTT should be done in the morning after an overnight fast of between 8 and 14 hours. During the three previous days the subject must have an unrestricted diet (containing at least 150 g carbohydrateCarbohydrate
A carbohydrate is an organic compound with the empirical formula ; that is, consists only of carbon, hydrogen, and oxygen, with a hydrogen:oxygen atom ratio of 2:1 . However, there are exceptions to this. One common example would be deoxyribose, a component of DNA, which has the empirical...
per day) and unlimited physical activity. The subject should remain seated during the test and should not smoke throughout the test.
The test involves drinking a solution containing a certain amount of glucose, and drawing blood to measure glucose levels at the start and on set time intervals thereafter.
The diagnostic criteria from the National Diabetes Data Group (NDDG) have been used most often, but some centers rely on the Carpenter and Coustan criteria, which set the cutoff for normal at lower values. Compared with the NDDG criteria, the Carpenter and Coustan criteria lead to a diagnosis of gestational diabetes in 54 percent more pregnant women, with an increased cost and no compelling evidence of improved perinatal outcomes.
The following are the values which the American Diabetes Association
American Diabetes Association
The American Diabetes Association is a United States-based association working to fight the consequences of diabetes, and to help those affected by diabetes...
considers to be abnormal during the 100 g of glucose OGTT:
- Fasting blood glucose level ≥95 mg/dl (5.33 mmol/L)
- 1 hour blood glucose level ≥180 mg/dl (10 mmol/L)
- 2 hour blood glucose level ≥155 mg/dl (8.6 mmol/L)
- 3 hour blood glucose level ≥140 mg/dl (7.8 mmol/L)
An alternative test uses a 75 g glucose load and measures the blood glucose levels before and after 1 and 2 hours, using the same reference values. This test will identify fewer women who are at risk, and there is only a weak concordance (agreement rate) between this test and a 3 hour 100 g test.
The glucose values used to detect gestational diabetes were first determined by O'Sullivan and Mahan (1964) in a retrospective cohort study
Retrospective cohort study
A retrospective cohort study, also called a historic cohort study, generally means to take a look back at events that already have taken place...
(using a 100 grams of glucose OGTT) designed to detect risk of developing type 2 diabetes in the future. The values were set using whole blood and required two values reaching or exceeding the value to be positive. Subsequent information led to alterations in O'Sullivan's criteria. When methods for blood glucose determination changed from the use of whole blood to venous plasma samples, the criteria for GDM were also changed.
Urinary glucose testing
Women with GDM may have high glucose levels in their urine (glucosuria). Although dipstickDipstick
A dipstick is one of several measurement devices.Some dipsticks are dipped into a liquid to perform a chemical test or to provide a measure of quantity of the liquid....
testing is widely practiced, it performs poorly, and discontinuing routine dipstick testing has not been shown to cause underdiagnosis where universal screening is performed. Increased glomerular filtration rates during pregnancy contribute to some 50% of women having glucose in their urine on dipstick tests at some point during their pregnancy. The sensitivity of glucosuria for GDM in the first 2 trimesters is only around 10% and the positive predictive value
Positive predictive value
In statistics and diagnostic testing, the positive predictive value, or precision rate is the proportion of subjects with positive test results who are correctly diagnosed. It is a critical measure of the performance of a diagnostic method, as it reflects the probability that a positive test...
is around 20%.
Management

Quality of life
The term quality of life is used to evaluate the general well-being of individuals and societies. The term is used in a wide range of contexts, including the fields of international development, healthcare, and politics. Quality of life should not be confused with the concept of standard of...
. Unfortunately, treatment of GDM is also accompanied by more infants admitted to neonatal wards and more inductions of labour, with no proven decrease in cesarean section rates or perinatal mortality
Perinatal mortality
Perinatal mortality , also perinatal death, refers to the death of a fetus or neonate and is the basis to calculate the perinatal mortality rate. Variations in the precise definition of the perinatal mortality exist specifically concerning the issue of inclusion or exclusion of early fetal and...
. These findings are still recent and controversial.
A repeat OGTT should be carried out 2–4 months after delivery, to confirm the diabetes has disappeared. Afterwards, regular screening for type 2 diabetes is advised.
If a diabetic diet
Diabetic diet
There is much controversy regarding what diet to recommend to sufferers of diabetes mellitus. The diet most often recommended is high in dietary fiber, especially soluble fiber, but low in fat . Recommendations of the fraction of total calories to be obtained from carbohydrate intake range from 1/6...
or G.I. Diet
G.I. Diet
The Low-Glycemic Index Diet was developed by Dr. David J. Jenkins, a professor of nutrition at the University of Toronto and later turned into a successful line of diet books by author and former president of the Heart and Stroke Foundation of Ontario, Rick Gallop. According to the publishing...
, exercise, and oral medication are inadequate to control glucose levels, insulin therapy may become necessary.
The development of macrosomia can be evaluated during pregnancy by using sonography
Obstetric ultrasonography
Obstetric sonography is the application of medical ultrasonography to obstetrics, in which sonography is used to visualize the embryo or foetus in its mother's uterus...
. Women who use insulin, with a history of stillbirth, or with hypertension are managed like women with overt diabetes.
Lifestyle
Counselling before pregnancy (for example, about preventive folic acidFolic acid
Folic acid and folate , as well as pteroyl-L-glutamic acid, pteroyl-L-glutamate, and pteroylmonoglutamic acid are forms of the water-soluble vitamin B9...
supplements) and multidisciplinary management are important for good pregnancy outcomes. Most women can manage their GDM with dietary changes and exercise. Self monitoring of blood glucose levels can guide therapy. Some women will need antidiabetic drugs, most commonly insulin
Insulin
Insulin is a hormone central to regulating carbohydrate and fat metabolism in the body. Insulin causes cells in the liver, muscle, and fat tissue to take up glucose from the blood, storing it as glycogen in the liver and muscle....
therapy.
Any diet needs to provide sufficient calories for pregnancy, typically 2,000 - 2,500 kcal with the exclusion of simple carbohydrates. The main goal of dietary modifications is to avoid peaks in blood sugar levels. This can be done by spreading carbohydrate intake over meals and snacks throughout the day, and using slow-release carbohydrate sources—known as the G.I. Diet
G.I. Diet
The Low-Glycemic Index Diet was developed by Dr. David J. Jenkins, a professor of nutrition at the University of Toronto and later turned into a successful line of diet books by author and former president of the Heart and Stroke Foundation of Ontario, Rick Gallop. According to the publishing...
. Since insulin resistance is highest in mornings, breakfast carbohydrates need to be restricted more. Ingesting more fiber in foods with whole grains, or fruit and vegetables can also reduce the risk of gestational diabetes.
Regular moderately intense physical exercise is advised, although there is no consensus on the specific structure of exercise programs for GDM.
Self monitoring can be accomplished using a handheld capillary glucose dosage system. Compliance with these glucometer systems can be low. Target ranges advised by the Australasian Diabetes in Pregnancy Society are as follows:
- fasting capillary blood glucose levels <5.5 mmol/L
- 1 hour postprandial capillary blood glucose levels <8.0 mmol/L
- 2 hour postprandial blood glucose levels <6.7 mmol/L
Regular blood samples can be used to determine HbA1c levels, which give an idea of glucose control over a longer time period.
Research suggests a possible benefit of breastfeeding
Breastfeeding
Breastfeeding is the feeding of an infant or young child with breast milk directly from female human breasts rather than from a baby bottle or other container. Babies have a sucking reflex that enables them to suck and swallow milk. It is recommended that mothers breastfeed for six months or...
to reduce the risk of diabetes and related risks for both mother and child.
Medication
If monitoring reveals failing control of glucose levels with these measures, or if there is evidence of complications like excessive fetal growth, treatment with insulin might become necessary. The most common therapeutic regime involves premeal fast-acting insulin to blunt sharp glucose rises after meals. Care needs to be taken to avoid low blood sugar levels (hypoglycemiaHypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
) due to excessive insulin injections. Insulin therapy can be normal or very tight; more injections can result in better control but requires more effort, and there is no consensus that it has large benefits.
There is some evidence that certain oral glycemic agents might be safe in pregnancy, or at least, are significantly less dangerous to the developing fetus than poorly controlled diabetes. Glyburide, a second generation sulfonylurea
Sulfonylurea
Sulfonylurea derivatives are a class of antidiabetic drugs that are used in the management of diabetes mellitus type 2. They act by increasing insulin release from the beta cells in the pancreas.-First generation:* Carbutamide...
, has been shown to be an effective alternative to insulin therapy. In one study, 4% of women needed supplemental insulin to reach blood sugar targets.
Metformin
Metformin
Metformin is an oral antidiabetic drug in the biguanide class. It is the first-line drug of choice for the treatment of type 2 diabetes, in particular, in overweight and obese people and those with normal kidney function. Its use in gestational diabetes has been limited by safety concerns...
has shown promising results, with its oral format being much more popular than insulin injections. Treatment of polycystic ovarian syndrome with metformin during pregnancy has been noted to decrease GDM levels. A recent randomized controlled trial
Randomized controlled trial
A randomized controlled trial is a type of scientific experiment - a form of clinical trial - most commonly used in testing the safety and efficacy or effectiveness of healthcare services or health technologies A randomized controlled trial (RCT) is a type of scientific experiment - a form of...
of metformin versus insulin showed that women preferred metformin tablets to insulin injections, and that metformin is safe and equally effective as insulin. Severe neonatal hypoglycemia was less common in insulin-treated women, but preterm delivery was more common. Almost half of patients did not reach sufficient control with metformin alone and needed supplemental therapy with insulin; compared to those treated with insulin alone, they required less insulin, and they gained less weight. With no long-term studies into children of women treated with the drug, here remains a possibility of long-term complications from metformin therapy, although follow-up at the age of 18 months of children born to women with polycystic ovarian syndrome and treated with metformin revealed no developmental abnormalities.
Prognosis
Gestational diabetes generally resolves once the baby is born. Based on different studies, the chances of developing GDM in a second pregnancy are between 30 and 84%, depending on ethnic background. A second pregnancy within 1 year of the previous pregnancy has a high rate of recurrence.Women diagnosed with gestational diabetes have an increased risk of developing diabetes mellitus in the future. The risk is highest in women who needed insulin treatment, had antibodies
Antibody
An antibody, also known as an immunoglobulin, is a large Y-shaped protein used by the immune system to identify and neutralize foreign objects such as bacteria and viruses. The antibody recognizes a unique part of the foreign target, termed an antigen...
associated with diabetes (such as antibodies against glutamate decarboxylase
Glutamate decarboxylase
Glutamate decarboxylase or glutamic acid decarboxylase is an enzyme that catalyzes the decarboxylation of glutamate to GABA and CO2. GAD uses PLP as a cofactor. The reaction proceeds as follows:...
, islet cell antibodies and/or insulinoma antigen-2), women with more than two previous pregnancies, and women who were obese (in order of importance). Women requiring insulin to manage gestational diabetes have a 50% risk of developing diabetes within the next five years. Depending on the population studied, the diagnostic criteria and the length of follow-up, the risk can vary enormously. The risk appears to be highest in the first 5 years, reaching a plateau thereafter. One of the longest studies followed a group of women from Boston, Massachusetts; half of them developed diabetes after 6 years, and more than 70% had diabetes after 28 years. In a retrospective study in Navajo
Navajo people
The Navajo of the Southwestern United States are the largest single federally recognized tribe of the United States of America. The Navajo Nation has 300,048 enrolled tribal members. The Navajo Nation constitutes an independent governmental body which manages the Navajo Indian reservation in the...
women, the risk of diabetes after GDM was estimated to be 50 to 70% after 11 years. Another study found a risk of diabetes after GDM of more than 25% after 15 years. In populations with a low risk for type 2 diabetes, in lean subjects and in patients with auto-antibodies
Autoimmunity
Autoimmunity is the failure of an organism to recognize its own constituent parts as self, which allows an immune response against its own cells and tissues. Any disease that results from such an aberrant immune response is termed an autoimmune disease...
, there is a higher rate of women developing type 1 diabetes.
Children of women with GDM have an increased risk for childhood and adult obesity and an increased risk of glucose intolerance and type 2 diabetes later in life. This risk relates to increased maternal glucose values. It is currently unclear how much genetic susceptibility and environmental factors each contribute to this risk, and if treatment of GDM can influence this outcome.
There are scarce statistical data on the risk of other conditions in women with GDM; in the Jerusalem Perinatal study, 410 out of 37962 patients were reported to have GDM, and there was a tendency towards more breast and pancreatic cancer, but more research is needed to confirm this finding.
Complications
GDM poses a risk to mother and child. This risk is largely related to high blood glucose levels and its consequences. The risk increases with higher blood glucose levels. Treatment resulting in better control of these levels can reduce some of the risks of GDM considerably.The two main risks GDM imposes on the baby are growth abnormalities and chemical imbalances after birth, which may require admission to a neonatal intensive care unit
Neonatal intensive care unit
A Neonatal Intensive Care Unit —also called a Special Care Nursery, newborn intensive care unit, intensive care nursery , and special care baby unit —is an intensive care unit specializing in the care of ill or premature newborn infants.The problem of premature and congenitally ill infants is not a...
. Infants born to mothers with GDM are at risk of being both large for gestational age
Large for gestational age
Large for gestational age is an indication of high prenatal growth rate, often defined as a weight that lies above the 90th percentile for that gestational age...
(macrosomic) and small for gestational age
Small for gestational age
Small for gestational age babies are those who are smaller in size than normal for the baby's sex and gestational age, most commonly defined as a weight below the 10th percentile for the gestational age.-Terminology:...
. Macrosomia in turn increases the risk of instrumental deliveries (e.g. forceps
Forceps
Forceps or forcipes are a handheld, hinged instrument used for grasping and holding objects. Forceps are used when fingers are too large to grasp small objects or when many objects need to be held at one time while the hands are used to perform a task. The term 'forceps' is used almost exclusively...
, ventouse
Ventouse
Ventouse is a vacuum device used to assist the delivery of a baby when the second stage of labour has not progressed adequately. It is an alternative to a forceps delivery and caesarean section. It cannot be used when the baby is in the breech position or for premature births. This technique is...
and caesarean section
Caesarean section
A Caesarean section, is a surgical procedure in which one or more incisions are made through a mother's abdomen and uterus to deliver one or more babies, or, rarely, to remove a dead fetus...
) or problems during vaginal delivery (such as shoulder dystocia
Shoulder dystocia
Shoulder dystocia is a specific case of dystocia whereby after the delivery of the head, the anterior shoulder of the infant cannot pass below the pubic symphysis, or requires significant manipulation to pass below the pubic symphysis. It is diagnosed when the shoulders fail to deliver shortly...
). Macrosomia may affect 12% of normal women compared to 20% of patients with GDM. However, the evidence for each of these complications is not equally strong; in the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study for example, there was an increased risk for babies to be large but not small for gestational age. Research into complications for GDM is difficult because of the many confounding factors (such as obesity). Labelling a woman as having GDM may in itself increase the risk of having a caesarean section.
Neonates are also at an increased risk of low blood glucose (hypoglycemia
Hypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
), jaundice
Jaundice
Jaundice is a yellowish pigmentation of the skin, the conjunctival membranes over the sclerae , and other mucous membranes caused by hyperbilirubinemia . This hyperbilirubinemia subsequently causes increased levels of bilirubin in the extracellular fluid...
, high red blood cell
Red blood cell
Red blood cells are the most common type of blood cell and the vertebrate organism's principal means of delivering oxygen to the body tissues via the blood flow through the circulatory system...
mass (polycythemia
Polycythemia
Polycythemia is a disease state in which the proportion of blood volume that is occupied by red blood cells increases...
) and low blood calcium (hypocalcemia) and magnesium (hypomagnesemia
Hypomagnesemia
Hypomagnesemia is an electrolyte disturbance in which there is an abnormally low level of magnesium in the blood. Usually a serum level less than 0.7 mmol/L is used as reference. The prefix hypo- means low . The middle 'magnes' refers to magnesium...
). GDM also interferes with maturation, causing dysmature babies prone to respiratory distress syndrome
Respiratory distress syndrome
There are two forms of respiratory distress syndrome:* ARDS, which is acute respiratory distress syndrome* Infant respiratory distress syndrome , which is a complication of premature birth, also known as hyaline membrane disease Also, respiratory distress can mean:* Shortness of breath*...
due to incomplete lung maturation and impaired surfactant
Surfactant
Surfactants are compounds that lower the surface tension of a liquid, the interfacial tension between two liquids, or that between a liquid and a solid...
synthesis.
Unlike pre-gestational diabetes, gestational diabetes has not been clearly shown to be an independent risk factor for birth defects. Birth defects usually originate sometime during the first trimester (before the 13th week) of pregnancy, whereas GDM gradually develops and is least pronounced during the first trimester. Studies have shown that the offspring of women with GDM are at a higher risk for congenital malformations. A large case-control study found that gestational diabetes was linked with a limited group of birth defects, and that this association was generally limited to women with a higher body mass index (≥ 25 kg/m²). It is difficult to make sure that this is not partially due to the inclusion of women with pre-existent type 2 diabetes who were not diagnosed before pregnancy.
Because of conflicting studies, it is unclear at the moment whether women with GDM have a higher risk of preeclampsia. In the HAPO study, the risk of preeclampsia was between 13% and 37% higher, although not all possible confounding factors were corrected.
Epidemiology
Gestational diabetes affects 3-10% of pregnancies, depending on the population studied.External links
- IDF Diabetes Atlas
- International Diabetes Federation
- National Institute of Child Health and Human Development - Am I at Risk for Gestational Diabetes?
- National Institute of Child Health and Human Development - Managing Gestational Diabetes: A Patient's Guide to a Healthy Pregnancy
- Gestational Diabetes Resource Guide - American Diabetes Association
- World Diabetes Day
- Diabetes.co.uk: Gestational Diabetes

