
Patient safety
Encyclopedia

Medical error
A medical error may be defined as a preventable adverse effect of care, whether or not it is evident or harmful to the patient. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, syndrome, behavior, infection, or other ailment.-Definitions:As a general...
that often leads to adverse healthcare events
Adverse effect (medicine)
In medicine, an adverse effect is a harmful and undesired effect resulting from a medication or other intervention such as surgery.An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. If it results from an unsuitable or incorrect dosage or...
. The frequency and magnitude of avoidable adverse patient events was not well known until the 1990s, when multiple countries reported staggering numbers of patients harmed and killed by medical errors. Recognizing that healthcare errors impact 1 in every 10 patients around the world, the World Health Organization
World Health Organization
The World Health Organization is a specialized agency of the United Nations that acts as a coordinating authority on international public health. Established on 7 April 1948, with headquarters in Geneva, Switzerland, the agency inherited the mandate and resources of its predecessor, the Health...
calls patient safety an endemic concern. Indeed, patient safety has emerged as a distinct healthcare discipline supported by an immature yet developing scientific framework. There is a significant transdisciplinary body of theoretical and research literature that informs the science of patient safety. The resulting patient safety knowledge continually informs improvement efforts such as: applying lessons learned from business and industry, adopting innovative technologies, educating providers and consumers, enhancing error reporting systems, and developing new economic incentives.
Prevalence of adverse events
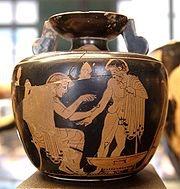
Hippocratic Oath
The Hippocratic Oath is an oath historically taken by physicians and other healthcare professionals swearing to practice medicine ethically. It is widely believed to have been written by Hippocrates, often regarded as the father of western medicine, or by one of his students. The oath is written in...
and pledged to "prescribe regimens for the good of my patients according to my ability and my judgment and never do harm to anyone."
Since then, the directive primum non nocere (“first do no harm) has become a central tenet for contemporary medicine. However, despite an increasing emphasis on the scientific basis of medical practice in Europe and the United States in the late 19th Century, data on adverse outcomes were hard to come by and the various studies commissioned collected mostly anecdotal events.
In the United States, the public and the medical specialty of anesthesia
Anesthesia
Anesthesia, or anaesthesia , traditionally meant the condition of having sensation blocked or temporarily taken away...
were shocked in April 1982 by the ABC
American Broadcasting Company
The American Broadcasting Company is an American commercial broadcasting television network. Created in 1943 from the former NBC Blue radio network, ABC is owned by The Walt Disney Company and is part of Disney-ABC Television Group. Its first broadcast on television was in 1948...
television program 20/20 entitled The Deep Sleep. Presenting accounts of anesthetic accidents, the producers stated that, every year, 6,000 Americans die or suffer brain damage related to these mishaps.
In 1983, the British Royal Society of Medicine
Royal Society of Medicine
The Royal Society of Medicine is a British charitable organisation whose main purpose is as a provider of medical education, running over 350 meetings and conferences each year.- History and overview :...
and the Harvard Medical School
Harvard Medical School
Harvard Medical School is the graduate medical school of Harvard University. It is located in the Longwood Medical Area of the Mission Hill neighborhood of Boston, Massachusetts....
jointly sponsored a symposium on anesthesia deaths and injuries, resulting in an agreement to share statistics and to conduct studies.
By 1984 the American Society of Anesthesiologists had established the Anesthesia Patient Safety Foundation. The APSF marked the first use of the term "patient safety" in the name of professional reviewing organization. Although anesthesiologists comprise only about 5% of physicians in the United States, anesthesiology became the leading medical specialty addressing issues of patient safety. Likewise in Australia, the Australian Patient Safety Foundation was founded in 1989 for anesthesia error monitoring. Both organizations were soon expanded as the magnitude of the medical error crisis became known.
To Err is Human

In the United States, the full magnitude and impact of errors in health care was not appreciated until the 1990s, when several reports brought attention to this issue.
In 1999, the Institute of Medicine
Institute of Medicine
The Institute of Medicine is a not-for-profit, non-governmental American organization founded in 1970, under the congressional charter of the National Academy of Sciences...
(IOM) of the National Academy of Sciences released a report, To Err is Human
To Err is Human
To Err is Human: Building a Safer Health System is a report issued in November 1999 by the U.S. Institute of Medicine that may have resulted in increased awareness of U.S. medical errors. The push for patient safety that followed its release continues...
: Building a Safer Health System.
The IOM called for a broad national effort to include establishment of a Center for Patient Safety, expanded reporting of adverse events, development of safety programs in health care organizations, and attention by regulators, health care purchasers, and professional societies. The majority of media attention, however, focused on the staggering statistics: from 44,000 to 98,000 preventable deaths annually due to medical error in hospitals, 7,000 preventable deaths related to medication errors alone. Within 2 weeks of the report's release, Congress began hearings and President Clinton ordered a government-wide study of the feasibility of implementing the report's recommendations.
Initial criticisms of the methodology in the IOM estimates focused on the statistical methods of amplifying low numbers of incidents in the pilot studies to the general population. However, subsequent reports emphasized the striking prevalence and consequences of medical error.
The experience has been similar in other countries.
- Ten years after a groundbreaking Australian study revealed 18,000 annual deaths from medical errors, Professor Bill Runciman, one of the study's authors and president of the Australian Patient Safety Foundation since its inception in 1989, reported himself a victim of a medical dosing error.
- The Department of Health Expert Group in June 2000 estimated that over 850,000 incidents harm National Health ServiceNational Health ServiceThe National Health Service is the shared name of three of the four publicly funded healthcare systems in the United Kingdom. They provide a comprehensive range of health services, the vast majority of which are free at the point of use to residents of the United Kingdom...
hospital patients in the United KingdomUnited KingdomThe United Kingdom of Great Britain and Northern IrelandIn the United Kingdom and Dependencies, other languages have been officially recognised as legitimate autochthonous languages under the European Charter for Regional or Minority Languages...
each year. On average forty incidents a year contribute to patient deaths in each NHS institution. - In 2004, the Canadian Adverse Events Study found that adverse events occurred in more than 7% of hospital admissions, and estimated that 9,000 to 24,000 Canadians die annually after an avoidable medical error.
- These and other reports from New Zealand, Denmark and developing countries have led the World Health OrganizationWorld Health OrganizationThe World Health Organization is a specialized agency of the United Nations that acts as a coordinating authority on international public health. Established on 7 April 1948, with headquarters in Geneva, Switzerland, the agency inherited the mandate and resources of its predecessor, the Health...
to estimate that one in ten persons receiving health care will suffer preventable harm.
Causes of healthcare error
- See also Healthcare error and Healthcare error proliferation modelHealthcare error proliferation modelThe Healthcare Error Proliferation Model is an adaptation of James Reason’s Swiss Cheese Model designed to illustrate the complexity inherent in the contemporary healthcare delivery system and the attribution of human error within these systems. The Healthcare Error Proliferation Model explains...
The simplest definition of a health care error is a preventable adverse effect
Adverse effect (medicine)
In medicine, an adverse effect is a harmful and undesired effect resulting from a medication or other intervention such as surgery.An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. If it results from an unsuitable or incorrect dosage or...
of care, whether or not it is evident or harmful to the patient. Errors have been, in part, attributed to:
Human Factors
- Variations in healthcare provider training & experience, fatigue, depression and burnout.
- Diverse patients, unfamiliar settings, time pressures.
- Failure to acknowledge the prevalence and seriousness of medical errors.
Medical complexity
- Complicated technologies, powerful drugs.
- Intensive care, prolonged hospital stay.
System failures
- Poor communication, unclear lines of authority of physicians, nurses, and other care providers.
- Complications increase as patient to nurse staffing ratio increases.
- Disconnected reporting systems within a hospital: fragmented systems in which numerous hand-offs of patients results in lack of coordination and errors.
- Drug names that look alike or sound alike.
- The impression that action is being taken by other groups within the institution.
- Reliance on automated systems to prevent error.
- Inadequate systems to share information about errors hamper analysis of contributory causes and improvement strategies.
- Cost-cutting measures by hospitals in response to reimbursement cutbacks.
- Environment and design factors. In emergencies, patient care may be rendered in areas poorly suited for safe monitoring. The American Institute of Architects has identified concerns for the safe design and construction of health care facilities.
- Infrastructure failure. According to the WHOWhoWho may refer to:* Who , an English-language pronoun* who , a Unix command* Who?, one of the Five Ws in journalism- Art and entertainment :* Who? , a 1958 novel by Algis Budrys...
, 50% of medical equipment in developing countries is only partly usable due to lack of skilled operators or parts. As a result, diagnostic procedures or treatments cannot be performed, leading to substandard treatment.
The Joint Commission's Annual Report on Quality and Safety 2007 found that inadequate communication between healthcare providers, or between providers and the patient and family members, was the root cause of over half the serious adverse events in accredited hospitals. Other leading causes included inadequate assessment of the patient's condition, and poor leadership or training.
Common misconceptions about adverse events are:
- "'Bad apples' or incompetent health care providers are a common cause." Many of the errors are normal human slips or lapses, and not the result of poor judgment or recklessness.
- "High risk procedures or medical specialties are responsible for most avoidable adverse events". Although some mistakes, such as in surgery, are easier to notice, errors occur in all levels of care. Even though complex procedures entail more risk, adverse outcomes are not usually due to error, but to the severity of the condition being treated. However, USPUnited States PharmacopeiaThe United States Pharmacopeia is the official pharmacopeia of the United States, published dually with the National Formulary as the USP-NF. The United States Pharmacopeial Convention is the nonprofit organization that owns the trademark and copyright to the USP-NF and publishes it every year...
has reported that medication errors during the course of a surgical procedure are three times more likely to cause harm to a patient than those occurring in other types of hospital care. - "If a patient experiences an adverse event during the process of care, an error has occurred". Most medical care entails some level of risk, and there can be complications or side effects, even unforeseen ones, from the underlying condition or from the treatment itself.
Safety programs in industry
Aviation safety- In the United States, two organizations contribute to one of the world's lowest aviation accident rates. Mandatory accident investigation is carried out by the National Transportation Safety BoardNational Transportation Safety BoardThe National Transportation Safety Board is an independent U.S. government investigative agency responsible for civil transportation accident investigation. In this role, the NTSB investigates and reports on aviation accidents and incidents, certain types of highway crashes, ship and marine...
, while the Aviation Safety Reporting SystemAviation Safety Reporting SystemThe Aviation Safety Reporting System, or ASRS, is the US Federal Aviation Administration's voluntary system that allows pilots and other airplane crew members to confidentially report near misses and close calls in the interest of improving air safety...
receives voluntary reports to identify deficiencies and provide data for planning improvements. The latter system is confidential and provides reports back to stakeholders without regulatory action. Similarities and contrasts have been noted between the "cultures of safety" in medicine and aviation. Pilots and medical personnel operate in complex environments, interact with technology, and are subject to fatigue, stress, danger, and loss of life and prestige as a consequence of error. Given the enviable record of aviation in accident prevention, a similar medical adverse event system would include both mandatory (for severe incidents) and voluntary non-punitive reporting, teamwork training, feedback on performance and an institutional commitment to data collection and analysis. The Patient Safety Reporting System (PSRS) is a program modeled upon the Aviation Safety Reporting System and developed by the Department of Veterans AffairsUnited States Department of Veterans AffairsThe United States Department of Veterans Affairs is a government-run military veteran benefit system with Cabinet-level status. It is the United States government’s second largest department, after the United States Department of Defense...
(VA) and the National Aeronautics and Space Administration (NASA) to monitor patient safety through voluntary, confidential reports.
Near-miss reporting
- A near missNear miss (safety)See Close Call, for the 2002 film.A near miss is an unplanned event that did not result in injury, illness, or damage – but had the potential to do so. Only a fortunate break in the chain of events prevented an injury, fatality or damage; in other words, a miss that was nonetheless very near...
is an unplanned event that did not result in injury, illness, or damage - but had the potential to do so. Reporting of near misses by observers is an established error reduction technique in aviation, and has been extended to private industry, traffic safety and fire-rescue services with reductions in accidents and injury. AORNAORNThe Association of periOperative Registered Nurses , represents more than 41,000 registered nurses in the United States and abroad who facilitate the management, teaching and practice of perioperative nursing, or who are enrolled in nursing education or engaged in perioperative research...
, a US-based professional organization of perioperative registered nurses, has put in effect a voluntary near miss reporting system (SafetyNet), covering medication or transfusion reactions, communication or consent issues, wrong patient or procedures, communication breakdown or technology malfunctions. An analysis of incidents allows safety alerts to be issued to AORN members.
Limits of the industrial safety model
- Unintended consequenceUnintended consequenceIn the social sciences, unintended consequences are outcomes that are not the outcomes intended by a purposeful action. The concept has long existed but was named and popularised in the 20th century by American sociologist Robert K. Merton...
s may occur as improvements in safety are undertaken. It may not be possible to attain maximum safety goals in healthcare without adversely affecting patient care in other ways. An example is blood transfusion; in recent years, to reduce the risk of transmissible infection in the blood supply, donors with only a small probability of infection have been excluded. The result has been a critical shortage of blood for other lifesaving purposes, with a broad impact on patient care. Application of high-reliability theory and normal accident theory can help predict the organizational consequences of implementing safety measures.
Technology in Healthcare
OverviewAccording to a study by RAND Health, the U.S. healthcare system could save more than $81 billion annually, reduce adverse healthcare events, and improve the quality of care if health information technology
Health information technology
Health information technology provides the umbrella framework to describe the comprehensive management of health information across computerized systems and its secure exchange between consumers, providers, government and quality entities, and insurers...
(HIT) is widely adopted. The most immediate barrier to widespread adoption of technology is cost despite the patient benefit from better health, and payer benefit from lower costs. However, hospitals pay in both higher costs for implementation and potentially lower revenues (depending on reimbursement scheme) due to reduced patient length of stay. The benefits provided by technological innovations also give rise to serious issues with the introduction of new and previously unseen error types.
Types of Healthcare Technology
Handwritten reports or notes, manual order entry, non-standard abbreviations and poor legibility lead to substantial errors and injuries, according to the IOM (2000) report. The follow-up IOM report, Crossing the Quality Chasm: A New Health System for the 21st Century, advised rapid adoption of electronic patient records, electronic medication ordering, with computer- and internet-based information systems to support clinical decisions. This section contains only the patient safety related aspects of HIT.Electronic Health Record (EHR)
The Electronic health record
Electronic Health Record
An electronic health record is an evolving concept defined as a systematic collection of electronic health information about individual patients or populations...
(EHR), previously known as the Electronic medical record
Electronic medical record
An electronic medical record is a computerized medical record created in an organization that delivers care, such as a hospital or physician's office...
(EMR), reduces several types of errors, including those related to prescription drugs, to emergent and preventive care, and to tests and procedures. Important features of modern EHR include automated drug-drug/drug-food interaction checks and allergy checks, standard drug dosages and patient education information. Also, these systems provide recurring alerts to remind clinicians of intervals for preventive care and to track referrals and test results. Clinical guidelines for disease management have a demonstrated benefit when accessible within the electronic record during the process of treating the patient. Advances in health informatics
Health informatics
.Health informatics is a discipline at the intersection of information science, computer science, and health care...
and widespread adoption of interoperable electronic health records promise access to a patient's records at any health care site. Still, there may be a weak link because of physicians' deficiencies in understanding the patient safety features of e.g. government approved software.
Portable offline emergency medical record devices have been developed to provide access to health records during widespread or extended infrastructure failure, such as in natural disasters or regional conflicts.
Active RFID platform
These systems' basic security measures are based on sound identifying electronic tags, in order that the patient details provided in different situations are always reliable. These systems offer three differently qualified options:
- Identification upon request of health care personnel, using scanners (similar to readers for passive RFID tags or scanners for barcode labels) to identify patient semi-automatically upon presentation of patient with tag to staff
- Automatic identification upon entry of patient. An automatic identification check is carried out on each person with tags (primarily patients) entering the area to determine the presented patient in contrast to other patient eralier entered into reach of the used reader.
- Automatic identification and range estimation upon approach to most proximate patient, excluding reads from more distant tags of other patients in the same area
Any of these options may be applied whenever and wherever patient details are required in electronic form Such identifying is essential when the information concerned is critical. There are increasing numbers of hospitals that have an RFID system to identify patients, for instance: Hospital La Fe in Valencia(Spain); Wayne Memorial Hospital (USA); Royal Alexandria Hospital (UK).
Computerized Provider Order Entry (CPOE)
Prescribing errors are the largest identified source of preventable errors in hospitals (IOM, 2000; 2007). The IOM (2006) estimates that each hospitalized patient, on average, is exposed to one medication error each day. Computerized provider order entry (CPOE), formerly called computer physician order entry
Computer physician order entry
Computerized physician order entry is a process of electronic entry of medical practitioner instructions for the treatment of patients under his or her care...
, can reduce medication errors by 80% overall but more importantly decrease harm to patients by 55%. A Leapfrog (2004) survey found that 16% of US clinics, hospitals, and medical practices are expected to utilize CPOE within 2 years.
Complete Safety Medication System
A standardized bar code system for dispensing drugs might prevent 25% of drug errors. Despite ample evidence to reduce medication errors, compete medication delivery systems (barcoding and Electronic prescribing
Electronic prescribing
Electronic prescribing or e-prescribing is the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of...
) have slow adoption by doctors and hospitals in the United States, due to concern with interoperability and compliance with future national standards. Such concerns are not inconsequential; standards for electronic prescribing for Medicare Part D
Medicare Part D
Medicare Part D is a federal program to subsidize the costs of prescription drugs for Medicare beneficiaries in the United States. It was enacted as part of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 and went into effect on January 1, 2006.- Eligibility and...
conflict with regulations in many US states.
Technological Iatrogenesis
Technology induced errors are significant and increasingly more evident in care delivery systems.This idiosyncratic and potentially serious problems associated with HIT implementation has recently become a tangible concern for healthcare and information technology professionals. As such, the term technological iatrogenesis describes this new category of adverse events that are an emergent property resulting from technological innovation creating system and microsystem disturbances. Healthcare systems are complex and adaptive, meaning there are many networks and connections working simultaneously to produce certain outcomes. When these systems are under the increased stresses caused by the diffusion of new technology, unfamiliar and new process errors often result. If not recognized, over time these new errors can collectively lead to catastrophic system failures. The term "e-iatrogenesis" can be used to describe the local error manifestation. The sources for these errors include:
- Prescriber and staff inexperience may lead to a false sense of security; that when technology suggests a course of action, errors are avoided.
- Shortcut or default selections can override non-standard medication regimens for elderly or underweight patients, resulting in toxic doses.
- CPOE and automated drug dispensing was identified as a cause of error by 84% of over 500 health care facilities participating in a surveillance system by the United States Pharmacopoeia.
- Irrelevant or frequent warnings can interrupt work flow.
Solutions include ongoing changes in design to cope with unique medical settings, supervising overrides from automatic systems, and training (and re-training) all users.
Evidence-based medicine

Evidence-based medicine
Evidence-based medicine
Evidence-based medicine or evidence-based practice aims to apply the best available evidence gained from the scientific method to clinical decision making. It seeks to assess the strength of evidence of the risks and benefits of treatments and diagnostic tests...
integrates an individual doctor's exam and diagnostic skills for a specific patient, with the best available evidence from medical research. The doctor's expertise includes both diagnostic skills and consideration of individual patient's rights and preferences in making decisions about his or her care. The clinician uses pertinent clinical research on the accuracy of diagnostic tests and the efficacy and safety of therapy, rehabilitation, and prevention to develop an individual plan of care. The development of evidence-based recommendations for specific medical conditions, termed clinical practice guidelines
Guideline (medical)
A medical guideline is a document with the aim of guiding decisions and criteria regarding diagnosis, management, and treatment in specific areas of healthcare...
or "best practices", has accelerated in the past few years. In the United States, over 1,700 guidelines (see example image, right) have been developed as a resource for physicians to apply to specific patient presentations. The National Institute for Health and Clinical Excellence (NICE) in the United Kingdom provides detailed "clinical guidance" for both health care professionals and the public about specific medical conditions. National Guideline Agencies from all continents collaborate in the Guidelines International Network
Guidelines International Network
The Guidelines International Network is an international scientific asssociation of organisations and individuals interested and involved in development and application of evidence based guidelines and health care information...
, which entertains the largest guideline library worldwide.
Advantages:
- Evidence-based medicine may reduce adverse events, especially those involving incorrect diagnosis, outdated or risky tests or procedures, or medication overuse.
- Clinical guidelines provide a common framework for improving communication among clinicians, patients and non-medical purchasers of health care.
- Errors related to changing shifts or multiple specialists are reduced by a consistent plan of care.
- Information on the clinical effectiveness of treatments and services can help providers, consumers and purchasers of health care make better use of limited resources.
- As medical advances become available, doctors and nurses can keep up with new tests and treatments as guidelines are improved.
Drawbacks:
- Managed care plans may attempt limit "unnecessary" services to cut the costs of health care, despite evidence that guidelines are not designed for general screening, rather as decision-making tools when an individual practitioner evaluates a specific patient.
- The medical literature is evolving and often controversial; development of guidelines requires consensus.
- Implementing guidelines and educating the entire health care team within a facility costs time and resources (which may be recovered by future efficiency and error reduction).
- Clinicians may resist evidence-based medicine as a threat to traditional relationships between patients, doctors and other health professionals, since any participant can influence decisions.
- Failing to follow guidelines might increase the risk of liabilityMedical malpracticeMedical malpractice is professional negligence by act or omission by a health care provider in which the treatment provided falls below the accepted standard of practice in the medical community and causes injury or death to the patient, with most cases involving medical error. Standards and...
or disciplinary action by regulators.
Quality and safety initiatives in community pharmacy practice
Community pharmacy practice is making important advances in the quality and safety movement despite the limited number of federal and state regulations that exist and in the absence of national accreditation organizations such as the Joint Commission - a driving force for performance improvement in health care systems. Community pharmacies are using automated drug dispensing devices (robots), computerized drug utilization review tools, and most recently, the ability to receive electronic prescriptions from prescribers to decrease the risk for error and increase the likelihood of delivering high quality of care.Quality Assurance (QA) in community practice is a relatively new concept. , only 16 states have some form of legislation that regulates QA in community pharmacy practice. While most state QA legislation focuses on error reduction, North Carolina has recently approved legislation that requires the pharmacy QA program to include error reduction strategies and assessments of the quality of their pharmaceutical care outcomes and pharmacy services.
Health literacy
Health literacyHealth literacy
Health literacy is an individual's ability to read, understand and use healthcare information to make decisions and follow instructions for treatment...
is a common and serious safety concern. A study of 2,600 patients at two hospitals determined that between 26-60% of patients could not understand medication directions, a standard informed consent
Informed consent
Informed consent is a phrase often used in law to indicate that the consent a person gives meets certain minimum standards. As a literal matter, in the absence of fraud, it is redundant. An informed consent can be said to have been given based upon a clear appreciation and understanding of the...
, or basic health care materials. This mismatch between a clinician's level of communication and a patient's ability to understand can lead to medication errors and adverse outcomes.
The Institute of Medicine
Institute of Medicine
The Institute of Medicine is a not-for-profit, non-governmental American organization founded in 1970, under the congressional charter of the National Academy of Sciences...
(2004) report found low health literacy levels negatively affects healthcare outcomes. In particular, these patients have a higher risk of hospitalization and longer hospital stays, are less likely to comply with treatment, are more likely to make errors with medication, and are more ill when they seek medical care.
Pay for performance (P4P)
Pay for performance systems link compensation to measures of work quality or goals. , 75 percent of all U.S. companies connect at least part of an employee's pay to measures of performance, and in healthcare, over 100 private and federal pilot programs are underway. Current methods of healthcare payment may actually reward less-safe care, since some insurance companies will not pay for new practices to reduce errors, while physicians and hospitals can bill for additional services that are needed when patients are injured by mistakes. However, early studies showed little gain in quality for the money spent, as well as evidence suggesting unintended consequences, like the avoidance of high-risk patients, when payment was linked to outcome improvements. The 2006 Institute of Medicine report Preventing Medication Errors recommended "incentives...so that profitability of hospitals, clinics, pharmacies, insurance companies, and manufacturers (are) aligned with patient safety goals;...(to) strengthen the business case for quality and safety."There is widespread international interest in health care pay-for-performance programs in a range of countries, including the United Kingdom, United States, Australia, Canada, Germany, the Netherlands, and New Zealand.
United Kingdom
In the United Kingdom, the National Health ServiceNational Health Service
The National Health Service is the shared name of three of the four publicly funded healthcare systems in the United Kingdom. They provide a comprehensive range of health services, the vast majority of which are free at the point of use to residents of the United Kingdom...
(NHS) began an ambitious pay for performance initiative in 2004, known as the Quality and Outcomes Framework (QOF). General practitioners agreed to increases in existing income according to performance with respect to 146 quality indicators covering clinical care for 10 chronic diseases, organization of care, and patient experience. Unlike proposed quality incentive programs in the United States, funding for primary care was increased 20% over previous levels. This allowed practices to invest in extra staff and technology; 90% of general practitioner
General practitioner
A general practitioner is a medical practitioner who treats acute and chronic illnesses and provides preventive care and health education for all ages and both sexes. They have particular skills in treating people with multiple health issues and comorbidities...
s use the NHS Electronic Prescription Service, and up to 50% use electronic health record
Electronic Health Record
An electronic health record is an evolving concept defined as a systematic collection of electronic health information about individual patients or populations...
s for the majority of clinical care. Early analysis showed that substantially increasing physicians' pay based on their success in meeting quality performance measures is successful. The 8,000 family practitioners included in the study earned an average of $40,000 more by collecting nearly 97% of the points available.
A component of this program, known as exception reporting, allows physicians to use criteria to exclude individual patients from the quality calculations that determine physician reimbursement. There was initial concern that exception reporting would allow inappropriate exclusion of patients in whom targets were missed ("gaming"). However, a 2008 study has shown little evidence of widespread gaming.
United States
In the United States, MedicareMedicare (United States)
Medicare is a social insurance program administered by the United States government, providing health insurance coverage to people who are aged 65 and over; to those who are under 65 and are permanently physically disabled or who have a congenital physical disability; or to those who meet other...
has various pay-for-performance ("P4P") initiatives in offices, clinics and hospitals, seeking to improving quality and avoid unnecessary health care costs. The Centers for Medicare and Medicaid Services
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services , previously known as the Health Care Financing Administration , is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state governments to administer...
(CMS) has several demonstration projects underway offering compensation for improvements:
- Payments for better care coordination between home, hospital and offices for patients with chronic illnesses. In April 2005, CMS launched its first value-based purchasing pilot or "demonstration" project- the three-year Medicare Physician Group Practice (PGP) Demonstration. The project involves ten large, multi-specialty physician practices caring for more than 200,000 Medicare fee-for-service beneficiaries. Participating practices will phase in quality standards for preventive care and the management of common chronic illnesses such as diabetes. Practices meeting these standards will be eligible for rewards from savings due to resulting improvements in patient management. The First Evaluation Report to Congress in 2006 showed that the model rewarded high quality, efficient provision of health care, but the lack of up-front payment for the investment in new systems of case management "have made for an uncertain future with respect for any payments under the demonstration."
- A set of 10 hospital quality measures which, if reported to CMS, will increase the payments that hospitals receive for each discharge. By the third year of the demonstration, those hospitals that do not meet a threshold on quality will be subject to reductions in payment. Preliminary data from the second year of the study indicates that pay for performance was associated with a roughly 2.5% to 4.0% improvement in compliance with quality measures, compared with the control hospitals. Dr. Arnold Epstein of the Harvard School of Public Health commented in an accompanying editorial that pay-for-performance "is fundamentally a social experiment likely to have only modest incremental value." Unintended consequences of some publicly reported hospital quality measures have adversely affected patient care. The requirement to give the first antibiotic dose in the emergency department within 4 hours, if the patient has pneumonia, has caused an increase in pneumonia misdiagnosis.
- Rewards to physicians for improving health outcomes by the use of health information technologyHealth informatics.Health informatics is a discipline at the intersection of information science, computer science, and health care...
in the care of chronically ill Medicare patients.
- Disincentives: The Tax Relief & Health Care Act of 2006 required the HHSHHS-Medicine:*Hyperglycemic hyperosmolar state, a complication of diabetes-Individual high schools:*Hackensack High School - Hackensack, New Jersey, US*Hackettstown High School - Hackettstown, New Jersey, US*Hadleigh High School - Hadleigh, Suffolk, England...
Inspector General to study ways that Medicare payments to hospitals could be recouped for "never events", as defined by the National Quality Forum, including hospital infections. In August 2007, CMS announced that it will stop payments to hospitals for several negative consequences of care that result in injury, illness or death. This rule, effective October 2008, would reduce hospital payments for eight serious types of preventable incidents: objects left in a patient during surgery, blood transfusion reaction, air embolismAir embolismAn air embolism, or more generally gas embolism, is a pathological condition caused by gas bubbles in a vascular system. The most common context is a human body, in which case it refers to gas bubbles in the bloodstream...
, falls, mediastinitisMediastinitisMediastinitis is inflammation of the tissues in the mid-chest, or mediastinum. It can be either acute or chronic.Acute mediastinitis is usually bacterial and due to rupture of organs in the mediastinum. As the infection can progress rapidly, this is considered a serious condition...
, urinary tract infections from catheters, pressure ulcer, and sepsisSepsisSepsis is a potentially deadly medical condition that is characterized by a whole-body inflammatory state and the presence of a known or suspected infection. The body may develop this inflammatory response by the immune system to microbes in the blood, urine, lungs, skin, or other tissues...
from catheters. Reporting of "never events" and creation of performance benchmarks for hospitals are also mandated. Other private health payers are considering similar actions; in 2005, HealthPartners, a Minnesota health insurer, chose not to cover 27 types of "never events". The Leapfrog Group has announced that will work with hospitals, health plans and consumer groups to advocate reducing payment for "never events", and will recognize hospitals that agree to certain steps when a serious avoidable adverse event occurs in the facility, including notifying the patient and patient safety organizationPatient safety organizationA patient safety organization is a group, institution or association that improves medical care by reducing medical errors. In the 1990s, reports in several countries revealed a staggering number of patient injuries and deaths each year due to avoidable adverse health care events...
s, and waiving costs. Physician groups involved in the management of complications, such as the Infectious Diseases Society of America, have voiced objections to these proposals, observing that "some patients develop infections despite application of all evidence-based practices known to avoid infection", and that a punitive response may discourage further study and slow the dramatic improvements that have already been made.
Complex illness
Pay for performance programs often target patients with serious and complex illnesses; such patients commonly interact with multiple healthcare providers and facilities. However, pilot programs now underway focus on simple indicators such as improvement in lab values or use of emergency services, avoiding areas of complexity such as multiple complications or several treating specialists. A 2007 study analyzing Medicare beneficiaries' healthcare visits showed that a median of two primary care physicians and five specialists provide care for a single patient. The authors doubt that pay-for-performance systems can accurately attribute responsibility for the outcome of care for such patients. The American College of Physicians Ethics has stated concerns about using a limited set of clinical practice parameters to assess quality, "especially if payment for good performance is grafted onto the current payment system, which does not reward robust comprehensive care...The elderly patient with multiple chronic conditions is especially vulnerable to this unwanted effect of powerful incentives." Present pay-for-performance systems measure good performance based on specified clinical measurements, such as glycohemoglobin for diabetic patients. Healthcare providers who are monitored by such limited criteria have a powerful incentive to deselect (dismiss or refuse to accept) patients whose outcome measures fall below the quality standard and therefore worsen the provider's assessment. Patients with low health literacy, inadequate financial resources to afford expensive medications or treatments, and ethnic groups traditionally subject to healthcare inequities may also be deselected by providers seeking improved performance measures.Mandatory reporting
Denmark :The Danish Act on Patient Safety passed Parliament in June 2003, and on January 1, 2004 Denmark became the first country to introduce nation-wide mandatory reporting. The Act obligates frontline personnel to report adverse events to a national reporting system. Hospital owners are obligated to act on the reports and the National Board of Health is obligated to communicate the learning nationally. The reporting system is intended purely for learning and frontline personnel cannot experience sanctions for reporting. This is stated in Section 6 of the Danish Act on Patient Safety (as of January 1, 2007: Section 201 of the Danish Health Act): "A frontline person who reports an adverse event cannot as a result of that report be subjected to investigation or disciplinary action from the employer, the Board of Health or the Court of Justice." The reporting system and the Danish Patient Safety Database is described in further detail in a National Board of Health publication.United Kingdom :The National Patient Safety Agency encourages voluntary reporting of health care errors, but has several specific instances, known as "Confidential Enquiries", for which investigation is routinely initiated: maternal or infant deaths, childhood deaths to age 16, deaths in persons with mental illness, and perioperative and unexpected medical deaths. Medical records and questionnaires are requested from the involved clinician, and participation has been high, since individual details are confidential.
United States :The 1999 Institute of Medicine (IOM) report recommended "a nationwide mandatory reporting system … that provides for … collection of standardized information by state governments about adverse events that result in death or serious harm." Professional organizations, such as the Anesthesia Patient Safety Foundation, responded negatively: "Mandatory reporting systems in general create incentives for individuals and institutions to play a numbers game. If such reporting becomes linked to punitive action or inappropriate public disclosure, there is a high risk of driving reporting "underground", and of reinforcing the cultures of silence and blame that many believe are at the heart of the problems of medical error…"
- Although 23 states established mandatory reporting systems for serious patient injuries or death by 2005, the national database envisioned in the IOM report was delayed by the controversy over mandatory versus voluntary reporting. Finally in 2005, the US Congress passed the long-debated Patient Safety and Quality Improvement Act, establishing a federal reporting database. Hospitals reports of serious patient harm are voluntary, collected by patient safety organizationPatient safety organizationA patient safety organization is a group, institution or association that improves medical care by reducing medical errors. In the 1990s, reports in several countries revealed a staggering number of patient injuries and deaths each year due to avoidable adverse health care events...
s under contract to analyze errors and recommend improvements. The federal government serves to coordinate data collection and maintain the national database. Reports remain confidential, and cannot be used in liability cases. Consumer groups have objected to the lack of transparency, claiming it denies the public information on the safety of specific hospitals.
Voluntary disclosure
In public surveys, a significant majority of those surveyed believe that health care providers should be required to report all serious medical errors publicly. However, reviews of the medical literature show little effect of publicly-reported performance data on patient safety or the quality of care. Public reporting on the quality of individual providers or hospitals does not seem to affect selection of hospitals and individual providers. Some studies have shown that reporting performance data stimulates quality improvement activity in hospitals.Medical error
Ethical standards of the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), the American Medical Association
American Medical Association
The American Medical Association , founded in 1847 and incorporated in 1897, is the largest association of medical doctors and medical students in the United States.-Scope and operations:...
(AMA) Council on Ethical and Judicial Affairs, and the American College of Physicians
American College of Physicians
The American College of Physicians is a national organization of doctors of internal medicine —physicians who specialize in the prevention, detection, and treatment of illnesses in adults. With 130,000 members, ACP is the largest medical-specialty organization and second-largest physician group in...
Ethics Manual require disclosure of the most serious adverse events. However, many doctors and hospitals do not report errors under the current system because of concerns about malpractice
Malpractice
In law, malpractice is a type of negligence in, which the professional under a duty to act, fails to follow generally accepted professional standards, and that breach of duty is the proximate cause of injury to a plaintiff who suffers harm...
lawsuits; this prevents collection of information needed to find and correct the conditions that lead to mistakes. , 35 US states have statutes allowing doctors and health care providers to apologize and offer expressions of regret without their words being used against them in court, and 7 states have also passed laws mandating written disclosure of adverse events and bad outcomes to patients and families. In September 2005, US Senators Clinton
Hillary Rodham Clinton
Hillary Diane Rodham Clinton is the 67th United States Secretary of State, serving in the administration of President Barack Obama. She was a United States Senator for New York from 2001 to 2009. As the wife of the 42nd President of the United States, Bill Clinton, she was the First Lady of the...
and Obama
Barack Obama
Barack Hussein Obama II is the 44th and current President of the United States. He is the first African American to hold the office. Obama previously served as a United States Senator from Illinois, from January 2005 until he resigned following his victory in the 2008 presidential election.Born in...
introduced the National Medical Error Disclosure and Compensation (MEDiC) Bill, providing physicians protection from liability and a safe environment for disclosure, as part of a program to notify and compensate patients harmed by medical errors. It is now the policy of several academic medical centers, including Johns Hopkins, University of Illinois and Stanford, to promptly disclose medical errors, offering apologies and compensation. This national initiative, hoping to restore integrity to dealings with patients, make it easier to learn from mistakes and avoid angry lawsuits, was modeled after a University of Michigan
University of Michigan
The University of Michigan is a public research university located in Ann Arbor, Michigan in the United States. It is the state's oldest university and the flagship campus of the University of Michigan...
Hospital System program that has reduced the number of lawsuits against the hospital by 75% and has decreased the average litigation cost. The Veterans Health Administration requires the disclosure of all adverse events to patients, even those that are not obvious. However, these initiatives have only included hospitals that are self-insured and that employ their staffs, thus limiting the number of parties involved.
Performance
In April 2008, consumer, employer and labor organizations announced an agreement with major physician organizations and health insurers on principles to measure and report doctors' performance on quality and cost.
United Kingdom
In the United Kingdom, whistleblowing is well recognised and is government sanctioned, as a way to protect patients by encouraging employees to call attention to deficient services. Health authorities are encouraged to put local policies in place to protect whistleblowers.
Studies of patient safety
Numerous organizations, government branches, and private companies conduct research studies to investigate the overall health of patient safety in America and across the globe. Despite the shocking and widely publicized statistics on preventable deaths due to medical errors in America's hospitals, the 2006 National Healthcare Quality Report assembled by the Agency for Healthcare Research and QualityAgency for Healthcare Research and Quality
The Agency for Healthcare Research and Quality is a part of the United States Department of Health and Human Services, which supports research designed to improve the outcomes and quality of health care, reduce its costs, address patient safety and medical errors, and broaden access to effective...
(AHRQ) had the following sobering assessment:
- Most measures of Quality are improving, but the pace of change remains modest.
- Quality improvement varies by setting and phase of care.
- The rate of improvement accelerated for some measures while a few continued to show deterioration.
- Variation in heath care quality remains high.
A 2011 study of more than 1,000 patients with advanced colon cancer found that one in eight was treated with at least one drug regimen with specific recommendations against their use in the National Comprehensive Cancer Network guidelines. The study focused on three chemotherapy regimens that were not supported by evidence from prior clinical studies or clinical practice guidelines. One treatment was rated "insufficient data to support," one had been "shown to be ineffective," and one was supported by "no data, nor is there a compelling rationale." Many of the patients received multiple cycles of non-beneficial chemotherapy and some received two or more unproven treatments. Potential side effects for the treatments include hypertension
Hypertension
Hypertension or high blood pressure is a cardiac chronic medical condition in which the systemic arterial blood pressure is elevated. What that means is that the heart is having to work harder than it should to pump the blood around the body. Blood pressure involves two measurements, systolic and...
, heightened risk of bleeding and bowel perforation.
Organizations advocating patient safety
Several authors of the 1999 Institute of Medicine report revisited the status of their recommendations and the state of patient safety, five years after "To Err is Human". Discovering that patient safety had become a frequent topic for journalists, health care experts, and the public, it was harder to see overall improvements on a national level. What was noteworthy was the impact on attitudes and organizations. Few health care professionals now doubted that preventable medical injuries were a serious problem. The central concept of the report—that bad systems and not bad people lead to most errors—became established in patient safety efforts. A broad array of organizations now advance the cause of patient safety. For instance, in 2010 the principal European anaesthesiology organisations launched The Helsinki Declaration for Patient Safety in AnaesthesiologyThe Helsinki Declaration for Patient Safety in Anaesthesiology
The Helsinki Declaration for Patient Safety in Anaesthesiology is a document prepared jointly by the two principal anaesthesiology organizations in Europe, The European Board of Anaesthesiology and the European Society of Anaesthesiology . It was launched in June 2010 at the Euroanaesthesia...
, which incorporates many of the principles described above.
See also
- Adverse effect (medicine)Adverse effect (medicine)In medicine, an adverse effect is a harmful and undesired effect resulting from a medication or other intervention such as surgery.An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. If it results from an unsuitable or incorrect dosage or...
- Adverse eventAdverse eventAn adverse event is any adverse change in health or side effect that occurs in a person who participates in a clinical trial while the patient is receiving the treatment or within a previously specified period of time after the treatment has been completed.AEs in patients participating in...
- Barcode technology in healthcareBarcode technology in healthcareBarcode technology in healthcare is the use of optical machine-readable representation of data in a hospital or healthcare setting.Dating back to the 1970s, there has been a continual effort among healthcare settings to adopt barcode technology. In the early 2000s, published reports began to...
- Blood transfusionBlood transfusionBlood transfusion is the process of receiving blood products into one's circulation intravenously. Transfusions are used in a variety of medical conditions to replace lost components of the blood...
- Classification of Pharmaco-Therapeutic ReferralsClassification of Pharmaco-Therapeutic ReferralsThe Classification of Pharmaco-Therapeutic Referrals is a taxonomy focused to define and group together situations requiring a referral from pharmacists to physicians regarding the pharmacotherapy used by the patients. It has been published in 2008...
- Compliance (medicine)Compliance (medicine)In medicine, compliance describes the degree to which a patient correctly follows medical advice...
- EudraVigilanceEudraVigilanceEudraVigilance is the European data processing network and management system for reporting and evaluation of suspected adverse reactions during the development of new drugs and for following the marketing authorisation of medicinal products in the European Economic Area .The European...
- Evidence-based medicineEvidence-based medicineEvidence-based medicine or evidence-based practice aims to apply the best available evidence gained from the scientific method to clinical decision making. It seeks to assess the strength of evidence of the risks and benefits of treatments and diagnostic tests...
- High 5s ProjectHigh 5s ProjectThe High 5s Project is an international patient safety collaborationlaunched by the World Health Organization in 2006.The project addresses concerns about patient safety around the world....
- Hospital accreditationHospital accreditationHospital accreditation has been defined as “A self-assessment and external peer assessment process used by health care organizations to accurately assess their level of performance in relation to established standards and to implement ways to continuously improve”...
- IatrogenesisIatrogenesisIatrogenesis, or an iatrogenic artifact is an inadvertent adverse effect or complication resulting from medical treatment or advice, including that of psychologists, therapists, pharmacists, nurses, physicians and dentists...
- Iatrogenic disorder
- Improvement Science Research NetworkImprovement Science Research NetworkThe ' is a large-scale practice based research network and coordinating center that was created to accelerate inter-professional improvement science in a systems context across multiple hospital sites...
- International healthcare accreditationInternational healthcare accreditationDue to the near-universal desire for quality healthcare, there is a growing interest in international healthcare accreditation. Providing healthcare, especially of an adequate standard, is a complex and challenging process...
- Inverse benefit lawInverse benefit lawThe Inverse Benefit Law states that the ratio of benefits to harms among patients taking new drugs tends to vary inversely with how extensively a drug is marketed...
- Medical ethicsMedical ethicsMedical ethics is a system of moral principles that apply values and judgments to the practice of medicine. As a scholarly discipline, medical ethics encompasses its practical application in clinical settings as well as work on its history, philosophy, theology, and sociology.-History:Historically,...
- Medical errorMedical errorA medical error may be defined as a preventable adverse effect of care, whether or not it is evident or harmful to the patient. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, syndrome, behavior, infection, or other ailment.-Definitions:As a general...
- Nosocomial infectionNosocomial infectionA nosocomial infection , also known as a hospital-acquired infection or HAI, is an infection whose development is favoured by a hospital environment, such as one acquired by a patient during a hospital visit or one developing among hospital staff...
- NursingNursingNursing is a healthcare profession focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life from conception to death....
- Patient safety organizationPatient safety organizationA patient safety organization is a group, institution or association that improves medical care by reducing medical errors. In the 1990s, reports in several countries revealed a staggering number of patient injuries and deaths each year due to avoidable adverse health care events...
- Patient Safety and NursingPatient safety and nursingNurses are knowledge workers whose main responsibility is to provide safe and effective care within constantly evolving health care systems. Nurses collaborate with one another, as well as doctors, aides, technicians, and others, to provide holistic care to patients...
- Patient Safety and Quality Improvement ActPatient Safety and Quality Improvement ActThe Patient Safety and Quality Improvement Act of 2005 : , 42 U.S.C. , established a system of patient safety organizations and a national patient safety database...
of 2005
- Palliative carePalliative carePalliative care is a specialized area of healthcare that focuses on relieving and preventing the suffering of patients...
- Peter PronovostPeter PronovostPeter J. Pronovost is an intensive care specialist physician at Johns Hopkins Hospital in Baltimore, Maryland.He is a Professor at the Johns Hopkins University School of Medicine in the Departments of Anesthesiology and Critical Care Medicine, and Surgery, Professor of Health Policy and Management...
- PharmacovigilancePharmacovigilancePharmacovigilance is the pharmacological science relating to the detection, assessment, understanding and prevention of adverse effects, particularly long term and short term side effects of medicines...
- Pharmacy Automation - The Tablet Counter
- Public healthPublic healthPublic health is "the science and art of preventing disease, prolonging life and promoting health through the organized efforts and informed choices of society, organizations, public and private, communities and individuals" . It is concerned with threats to health based on population health...
- Quaternary preventionQuaternary preventionThe quaternary prevention, concept coined by the Belgian general practitioner , are the action taken to identify patient at risk of overmedicalisation, to protect him from new medical invasion, and to suggest to him interventions, which are ethically acceptable...
- Serious adverse eventSerious adverse eventA serious adverse event in human drug trials are defined as any untowardmedical occurrence that at any dose#results in death,#is life-threatening#requires inpatient hospitalization or prolongation of existing hospitalization...
- Swiss Cheese modelSwiss Cheese modelModels of accident causation are used for the risk analysis and risk management of human systems. Since the 1990s they have gained widespread acceptance and use in healthcare, in the aviation safety industry, and in emergency service organizations...
of accident causation in human systems - Structured Clinical Interview for DSM-IVStructured Clinical Interview for DSM-IVThe Structured Clinical Interview for DSM-IV Axis I Disorders is a diagnostic exam used to determine DSM-IV Axis I disorders and Axis II disorders . There are at least 700 published studies in which the SCID was the diagnostic instrument used...
(SCID) - Unlicensed assistive personnelUnlicensed assistive personnelUnlicensed assistive personnel is an umbrella term to describe a job class of paraprofessionals who assist individuals with physical disabilities, mental impairments, and other health care needs with their activities of daily living and provide bedside care — including basic nursing...
External links
- CIMIT Center for Integration of Medicine and Innovative Technology - Nonprofit organizations together advocating for Patient safety
- Institute for safety in Office Based Surgery
- Health-EU Portal Patient Safety in the EU
- Academic Center for Evidence-Based Practice (ACE)
- Improvement Science Research Network (ISRN)

