
Anti-diabetic drug
Encyclopedia
Anti-diabetic medications treat diabetes mellitus
by lowering glucose
levels in the blood. With the exceptions of insulin
, exenatide
, and pramlintide
, all are administered orally and are thus also called oral hypoglycemic agents or oral antihyperglycemic agents. There are different classes of anti-diabetic drugs, and their selection depends on the nature of the diabetes, age and situation of the person, as well as other factors.
Diabetes mellitus type 1
is a disease caused by the lack of insulin. Insulin must be used in Type I, which must be injected.
Diabetes mellitus type 2
is a disease of insulin resistance by cells. Treatments include (1) agents which increase the amount of insulin secreted by the pancreas, (2) agents which increase the sensitivity of target organs to insulin, and (3) agents which decrease the rate at which glucose is absorbed from the gastrointestinal tract.
Several groups of drugs, mostly given by mouth, are effective in Type II, often in combination. The therapeutic combination in Type II may include insulin, not necessarily because oral agents have failed completely, but in search of a desired combination of effects. The great advantage of injected insulin in Type II is that a well-educated patient can adjust the dose, or even take additional doses, when blood glucose levels measured by the patient, usually with a simple meter, as needed by the measured amount of sugar in the blood.
, either by injections or by an insulin pump
. Research is underway of other routes of administration. In acute care settings, insulin may also be given intravenously. There are generally about four types of insulin, characterized by the rate which they are metabolized by the body.
.
s reduce hepatic
glucose output and increase uptake of glucose by the periphery, including skeletal muscle. Although it must be used with caution in patients with impaired liver or kidney
function, metformin
, a biguanide, has become the most commonly used agent for type 2 diabetes in children and teenagers. Amongst common diabetic drugs, metformin is the only widely used oral drug that does not cause weight gain.
Typical reduction in glycated hemoglobin (A1C) values for metformin is 1.5–2.0%.
Metformin is usually the first-line medication used for treatment of type 2 diabetes. It is generally prescribed at initial diagnosis in conjunction with exercise and weight loss as opposed to in the past, where it was prescribed after diet and exercise had failed. Initial dosing is 500 mg once daily, then if need be increased to 500 mg twice daily up to 1000 mg twice daily. It is also available in combination with other oral diabetic medications. There is an extended release formulation available, but it is typically reserved for patients experiencing GI side effects.
s (TZDs), also known as "glitazones," bind to PPARγ
, a type of nuclear regulatory protein involved in transcription of genes regulating glucose and fat metabolism. These PPARs act on peroxysome proliferator responsive elements (PPRE http://www.healthvalue.net/diabetesinsulinPPAR.html). The PPREs influence insulin sensitive genes, which enhance production of mRNAs of insulin-dependent enzymes. The final result is better use of glucose by the cells.
Typical reductions in glycated hemoglobin (A1C) values are 1.5–2.0%. Some examples are:
Multiple retrospective studies have resulted in a concern about rosiglitazone's safety, although it is established that the group, as a whole, has beneficial effects on diabetes. The greatest concern is an increase in the number of severe cardiac events in patients taking it. The ADOPT study showed initial therapy with drugs of this type may prevent the progression of disease, as did the DREAM trial.
Concerns about the safety of rosiglitazone arose when a retrospective meta-analysis was published in the New England Journal of Medicine. There have been a significant number of publications since then, and a Food and Drug Administration
panel voted, with some controversy, 20:3 that available studies "supported a signal of harm," but voted 22:1 to keep the drug on the market. The meta-analysis was not supported by an interim analysis of the trial designed to evaluate the issue, and several other reports have failed to conclude the controversy. This weak evidence for adverse effects has reduced the use of rosiglitazone, despite its important and sustained effects on glycemic control. Safety studies are continuing.
In contrast, at least one large prospective study, PROactive 05, has shown that pioglitazone
may decrease the overall incidence of cardiac events in people with type 2 diabetes who have already had a heart attack.
s were the first widely used oral anti-hyperglycaemic medications. They are insulin secretagogue
s, triggering insulin release by inhibiting the KATP channel of the pancreatic beta cell
s. Eight types of these pills have been marketed in North America, but not all remain available. The "second-generation" drugs are now more commonly used. They are more effective than first-generation drugs and have fewer side effects. All may cause weight gain.
Sulfonylureas bind strongly to plasma proteins. Sulfonylureas are only useful in Type II diabetes, as they work by stimulating endogenous release of insulin. They work best with patients over 40 years old, who have had diabetes mellitus for under ten years. They can not be used with type I diabetes, or diabetes of pregnancy. They can be safely used with metformin or -glitazones. The primary side effect is hypoglycemia
.
Typical reductions in glycated hemoglobin (A1C) values for second generation sulfonylureas are 1.0–2.0%.
s help the pancreas produce insulin and are often called "short-acting secretagogues." They act on the same potassium channels as sulfonylureas, but at a different binding site. By closing the potassium channels of the pancreatic beta cells, they open the calcium channels, hence enhancing insulin secretion.
They are taken with or shortly before meals to boost the insulin response to each meal. If a meal is skipped, the medication is also skipped.
Typical reductions in glycated hemoglobin (A1C) values are 0.5–1.0%.
Adverse reactions include weight gain and hypoglycemia.
s are "diabetes pills" but not technically hypoglycemic agents because they do not have a direct effect on insulin secretion or sensitivity. These agents slow the digestion of starch in the small intestine, so that glucose from the starch of a meal enters the bloodstream more slowly, and can be matched more effectively by an impaired insulin response or sensitivity. These agents are effective by themselves only in the earliest stages of impaired glucose tolerance
, but can be helpful in combination with other agents in type 2 diabetes.
Typical reductions in glycated hemoglobin (A1C) values are 0.5–1.0%.
These medications are rarely used in the United States because of the severity of their side effects (flatulence and bloating). They are more commonly prescribed in Europe. They do have the potential to cause weight loss by lowering the amount of sugar metabolized.
Research has shown the culinary mushroom maitake (Grifola frondosa
) has a hypoglycemic
effect, possibly due to the mushroom acting as a natural alpha glucosidase inhibitor.
s are insulin secretagogue
s. The two main candidate molecules that fulfill criteria for being an incretin are glucagon-like peptide-1
(GLP-1) and gastric inhibitory peptide (glucose-dependent insulinotropic peptide, GIP). Both GLP-1 and GIP are rapidly inactivated by the enzyme dipeptidyl peptidase-4
(DPP-4).
These agents may also cause a decrease in gastric motility, responsible for the common side effect of nausea, and is probably the mechanism by which weight loss occurs.
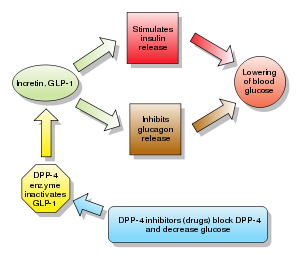
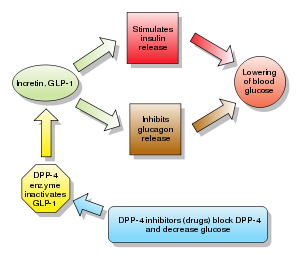
Dipeptidyl peptidase-4 (DPP-4) inhibitors
increase blood concentration of the incretin
GLP-1 by inhibiting its degradation by dipeptidyl peptidase-4
.
Examples are:
DPP-4 inhibitors lowered hemoglobin A1C values by 0.74%, comparable to other antidiabetic drugs.
In one RCT comprising 206 patients aged 65 or older (mean baseline HgbA1c of 7.8%) receiving either 50 or 100 mg/d of Sitagliptin
was shown to reduce HbA1c by 0.7% (combined result of both doses). A combined result of 5 RCTs enlisting a total of 279 patients aged 65 or older (mean baseline HbA1c of 8%) receiving 5 mg/d of Saxagliptin
was shown to reduce HbA1c by 0.73%. A combined result of 5 RCTs enlisting a total of 238 patients aged 65 or older (mean baseline HbA1c of 8.6%) receiving 100 mg/d of Vildagliptin
was shown to reduce HbA1c by 1.2%. Another set of 6 combined RCTs involving Alogliptin
(not yet approved, might be released in 2012) was shown to reduce HbA1c by 0.73% in 455 patients aged 65 or older who received 12.5 or 25 mg/d of the medication.
agonist analogues slow gastric emptying and suppress glucagon
. They have all the incretins actions except stimulation of insulin secretion. , pramlintide
is the only clinically available amylin analogue. Like insulin, it is administered by subcutaneous injection
. The most frequent and severe adverse effect of pramlintide is nausea
, which occurs mostly at the beginning of treatment and gradually reduces. Typical reductions in A1C values are 0.5–1.0%.
Most anti-diabetic agents are contraindicated in pregnancy, in which insulin is preferred.
has blood sugar lowering properties however whether or not it is useful for treating diabetes is unknown. While chromium supplements have no beneficial effect on healthy people, there might be an improvement in glucose metabolism in those with diabetics, although the evidence for this effect remains weak. Vanadyl sulfate, a salt of vanadium
, is still in preliminary studies. There is tentative research that thiamine
may prevent some diabetic complications however more research is needed.
Diabetes mellitus
Diabetes mellitus, often simply referred to as diabetes, is a group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin, or because cells do not respond to the insulin that is produced...
by lowering glucose
Glucose
Glucose is a simple sugar and an important carbohydrate in biology. Cells use it as the primary source of energy and a metabolic intermediate...
levels in the blood. With the exceptions of insulin
Insulin
Insulin is a hormone central to regulating carbohydrate and fat metabolism in the body. Insulin causes cells in the liver, muscle, and fat tissue to take up glucose from the blood, storing it as glycogen in the liver and muscle....
, exenatide
Exenatide
Exenatide is a medication approved in April 2005 for the treatment of diabetes mellitus type 2. It belongs to the group of incretin mimetics and is manufactured by Amylin Pharmaceuticals and Eli Lilly and Company....
, and pramlintide
Pramlintide
Pramlintide acetate is a relatively new adjunct for diabetes , developed by Amylin Pharmaceuticals.-Pharmacology:...
, all are administered orally and are thus also called oral hypoglycemic agents or oral antihyperglycemic agents. There are different classes of anti-diabetic drugs, and their selection depends on the nature of the diabetes, age and situation of the person, as well as other factors.
Diabetes mellitus type 1
Diabetes mellitus type 1
Diabetes mellitus type 1 is a form of diabetes mellitus that results from autoimmune destruction of insulin-producing beta cells of the pancreas. The subsequent lack of insulin leads to increased blood and urine glucose...
is a disease caused by the lack of insulin. Insulin must be used in Type I, which must be injected.
Diabetes mellitus type 2
Diabetes mellitus type 2
Diabetes mellitus type 2formerly non-insulin-dependent diabetes mellitus or adult-onset diabetesis a metabolic disorder that is characterized by high blood glucose in the context of insulin resistance and relative insulin deficiency. Diabetes is often initially managed by increasing exercise and...
is a disease of insulin resistance by cells. Treatments include (1) agents which increase the amount of insulin secreted by the pancreas, (2) agents which increase the sensitivity of target organs to insulin, and (3) agents which decrease the rate at which glucose is absorbed from the gastrointestinal tract.
Several groups of drugs, mostly given by mouth, are effective in Type II, often in combination. The therapeutic combination in Type II may include insulin, not necessarily because oral agents have failed completely, but in search of a desired combination of effects. The great advantage of injected insulin in Type II is that a well-educated patient can adjust the dose, or even take additional doses, when blood glucose levels measured by the patient, usually with a simple meter, as needed by the measured amount of sugar in the blood.
Insulin
Insulin is usually given subcutaneouslySubcutaneous tissue
The hypodermis, also called the hypoderm, subcutaneous tissue, or superficial fascia is the lowermost layer of the integumentary system in vertebrates. Types of cells that are found in the hypodermis are fibroblasts, adipose cells, and macrophages...
, either by injections or by an insulin pump
Insulin pump
The insulin pump is a medical device used for the administration of insulin in the treatment of diabetes mellitus, also known as continuous subcutaneous insulin infusion therapy.The device includes:...
. Research is underway of other routes of administration. In acute care settings, insulin may also be given intravenously. There are generally about four types of insulin, characterized by the rate which they are metabolized by the body.
Sensitizers
Insulin sensitizers address the core problem in Type II diabetes—insulin resistanceInsulin resistance
Insulin resistance is a physiological condition where the natural hormone insulin becomes less effective at lowering blood sugars. The resulting increase in blood glucose may raise levels outside the normal range and cause adverse health effects, depending on dietary conditions. Certain cell types...
.
Biguanides
BiguanideBiguanide
Biguanide can refer to a molecule, or to a class of drugs based upon this molecule. Biguanides can function as oral antihyperglycemic drugs used for diabetes mellitus or prediabetes treatment...
s reduce hepatic
Liver
The liver is a vital organ present in vertebrates and some other animals. It has a wide range of functions, including detoxification, protein synthesis, and production of biochemicals necessary for digestion...
glucose output and increase uptake of glucose by the periphery, including skeletal muscle. Although it must be used with caution in patients with impaired liver or kidney
Kidney
The kidneys, organs with several functions, serve essential regulatory roles in most animals, including vertebrates and some invertebrates. They are essential in the urinary system and also serve homeostatic functions such as the regulation of electrolytes, maintenance of acid–base balance, and...
function, metformin
Metformin
Metformin is an oral antidiabetic drug in the biguanide class. It is the first-line drug of choice for the treatment of type 2 diabetes, in particular, in overweight and obese people and those with normal kidney function. Its use in gestational diabetes has been limited by safety concerns...
, a biguanide, has become the most commonly used agent for type 2 diabetes in children and teenagers. Amongst common diabetic drugs, metformin is the only widely used oral drug that does not cause weight gain.
Typical reduction in glycated hemoglobin (A1C) values for metformin is 1.5–2.0%.
- MetforminMetforminMetformin is an oral antidiabetic drug in the biguanide class. It is the first-line drug of choice for the treatment of type 2 diabetes, in particular, in overweight and obese people and those with normal kidney function. Its use in gestational diabetes has been limited by safety concerns...
(Glucophage) may be the best choice for patients who also have heart failure, but it should be temporarily discontinued before any radiographic procedure involving intravenous iodinatedIodineIodine is a chemical element with the symbol I and atomic number 53. The name is pronounced , , or . The name is from the , meaning violet or purple, due to the color of elemental iodine vapor....
contrastRadiocontrastRadiocontrast agents are a type of medical contrast medium used to improve the visibility of internal bodily structures in an X-ray based imaging techniques such as computed tomography or radiography...
, as patients are at an increased risk of lactic acidosisLactic acidosisLactic acidosis is a physiological condition characterized by low pH in body tissues and blood accompanied by the buildup of lactate especially D-lactate, and is considered a distinct form of metabolic acidosis. The condition typically occurs when cells receive too little oxygen , for example...
. - PhenforminPhenforminPhenformin is an anti-diabetic drug from the biguanide class. It was marketed as DBI by Ciba-Geigy but was withdrawn from most markets in the late 1970s due to a high risk of lactic acidosis, which was fatal in 50% of cases....
(DBI) was used from 1960s through 1980s, but was withdrawn due to lactic acidosis risk. - BuforminBuforminBuformin is an oral anti-diabetic drug of the biguanide class, chemically related to metformin and phenformin. Buformin was marketed by German pharmaceutical company Grünenthal as Silubin.-Chemistry and Animal Toxicology:...
also was withdrawn due to lactic acidosis risk.
Metformin is usually the first-line medication used for treatment of type 2 diabetes. It is generally prescribed at initial diagnosis in conjunction with exercise and weight loss as opposed to in the past, where it was prescribed after diet and exercise had failed. Initial dosing is 500 mg once daily, then if need be increased to 500 mg twice daily up to 1000 mg twice daily. It is also available in combination with other oral diabetic medications. There is an extended release formulation available, but it is typically reserved for patients experiencing GI side effects.
Thiazolidinediones
ThiazolidinedioneThiazolidinedione
The thiazolidinediones , also known as glitazones, are a class of medications used in the treatment of diabetes mellitus type 2. They were introduced in the late 1990s.- Mechanism of action :...
s (TZDs), also known as "glitazones," bind to PPARγ
Peroxisome proliferator-activated receptor gamma
Peroxisome proliferator-activated receptor gamma , also known as the glitazone receptor, or NR1C3 is a type II nuclear receptor that in humans is encoded by the PPARG gene.Two isoforms of PPARG are detected in the human and in the mouse: PPAR-γ1 and...
, a type of nuclear regulatory protein involved in transcription of genes regulating glucose and fat metabolism. These PPARs act on peroxysome proliferator responsive elements (PPRE http://www.healthvalue.net/diabetesinsulinPPAR.html). The PPREs influence insulin sensitive genes, which enhance production of mRNAs of insulin-dependent enzymes. The final result is better use of glucose by the cells.
Typical reductions in glycated hemoglobin (A1C) values are 1.5–2.0%. Some examples are:
- rosiglitazoneRosiglitazoneRosiglitazone is an antidiabetic drug in the thiazolidinedione class of drugs. It works as an insulin sensitizer, by binding to the PPAR receptors in fat cells and making the cells more responsive to insulin...
(Avandia): the European Medicines AgencyEuropean Medicines AgencyThe European Medicines Agency is a European agency for the evaluation of medicinal products. From 1995 to 2004, the European Medicines Agency was known as European Agency for the Evaluation of Medicinal Products.Roughly parallel to the U.S...
recommended in September 2010 that it be suspended from the EU market due to elevated cardiovascular risks. - pioglitazonePioglitazonePioglitazone is a prescription drug of the class thiazolidinedione with hypoglycemic action.Pioglitazone is marketed as trademarks Actos in the USA, Canada, the UK and Germany, Glustin in Europe,"Glizone" and "Pioz" in India by Zydus CND and USV respectively and Zactos in Mexico by Takeda...
(Actos) - troglitazoneTroglitazoneTroglitazone is an anti-diabetic and antiinflammatory drug, and a member of the drug class of the thiazolidinediones. It was developed by Daiichi Sankyo Co.. In the United States, it was introduced and manufactured by Parke-Davis in the late 1990s, but turned out to be associated with an...
(Rezulin): used in 1990s, withdrawn due to hepatitisHepatitisHepatitis is a medical condition defined by the inflammation of the liver and characterized by the presence of inflammatory cells in the tissue of the organ. The name is from the Greek hepar , the root being hepat- , meaning liver, and suffix -itis, meaning "inflammation"...
and liver damage risk
Multiple retrospective studies have resulted in a concern about rosiglitazone's safety, although it is established that the group, as a whole, has beneficial effects on diabetes. The greatest concern is an increase in the number of severe cardiac events in patients taking it. The ADOPT study showed initial therapy with drugs of this type may prevent the progression of disease, as did the DREAM trial.
Concerns about the safety of rosiglitazone arose when a retrospective meta-analysis was published in the New England Journal of Medicine. There have been a significant number of publications since then, and a Food and Drug Administration
Food and Drug Administration
The Food and Drug Administration is an agency of the United States Department of Health and Human Services, one of the United States federal executive departments...
panel voted, with some controversy, 20:3 that available studies "supported a signal of harm," but voted 22:1 to keep the drug on the market. The meta-analysis was not supported by an interim analysis of the trial designed to evaluate the issue, and several other reports have failed to conclude the controversy. This weak evidence for adverse effects has reduced the use of rosiglitazone, despite its important and sustained effects on glycemic control. Safety studies are continuing.
In contrast, at least one large prospective study, PROactive 05, has shown that pioglitazone
Pioglitazone
Pioglitazone is a prescription drug of the class thiazolidinedione with hypoglycemic action.Pioglitazone is marketed as trademarks Actos in the USA, Canada, the UK and Germany, Glustin in Europe,"Glizone" and "Pioz" in India by Zydus CND and USV respectively and Zactos in Mexico by Takeda...
may decrease the overall incidence of cardiac events in people with type 2 diabetes who have already had a heart attack.
Sulfonylureas
SulfonylureaSulfonylurea
Sulfonylurea derivatives are a class of antidiabetic drugs that are used in the management of diabetes mellitus type 2. They act by increasing insulin release from the beta cells in the pancreas.-First generation:* Carbutamide...
s were the first widely used oral anti-hyperglycaemic medications. They are insulin secretagogue
Secretagogue
A secretagogue is a substance that causes another substance to be secreted. One example is gastrin,, which stimulates the H/K ATPase in the parietal cells...
s, triggering insulin release by inhibiting the KATP channel of the pancreatic beta cell
Beta cell
Beta cells are a type of cell in the pancreas located in the so-called islets of Langerhans. They make up 65-80% of the cells in the islets.-Function:...
s. Eight types of these pills have been marketed in North America, but not all remain available. The "second-generation" drugs are now more commonly used. They are more effective than first-generation drugs and have fewer side effects. All may cause weight gain.
Sulfonylureas bind strongly to plasma proteins. Sulfonylureas are only useful in Type II diabetes, as they work by stimulating endogenous release of insulin. They work best with patients over 40 years old, who have had diabetes mellitus for under ten years. They can not be used with type I diabetes, or diabetes of pregnancy. They can be safely used with metformin or -glitazones. The primary side effect is hypoglycemia
Hypoglycemia
Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"...
.
Typical reductions in glycated hemoglobin (A1C) values for second generation sulfonylureas are 1.0–2.0%.
- First-generation agents
- tolbutamideTolbutamideTolbutamide is a first generation potassium channel blocker, sulfonylurea oral hypoglycemic drug sold under the brand name Orinase. This drug may be used in the management of type II diabetes if diet alone is not effective. Tolbutamide stimulates the secretion of insulin by the pancreas...
(Orinase) - acetohexamideAcetohexamideAcetohexamide is a first-generation sulfonylurea medication used to treat diabetes mellitus type 2, particularly in people whose diabetes cannot be controlled by diet alone.-Mechanism of action:...
(Dymelor) - tolazamideTolazamideTolazamide is an oral blood glucose lowering drug used for people with Type 2 diabetes. It is part of the sulfonylurea family .-Synthesis:para-Toluenesulfonamide is converted to its carbamate with ethyl chloroformate in the presence of a base...
(Tolinase) - chlorpropamideChlorpropamideChlorpropamide is a drug in the sulphonylurea class used to treat type 2 diabetes mellitus. It is a long-acting sulphonylurea. It has more side effects than other sulphonylureas and its use is no longer recommended.-Mechanism of action:...
(Diabinese)
- tolbutamide
- Second-generation agents
- glipizideGlipizideGlipizide is an oral medium-to-long acting anti-diabetic drug from the sulfonylurea class. It is classified as a second generation sulfonylurea, which means that it undergoes enterohepatic circulation. The structure on the R2 group is a much larger cyclo or aromatic group compared to the 1st...
(Glucotrol) - glyburide (Diabeta, Micronase, Glynase)
- glimepirideGlimepirideGlimepiride is a medium-to-long acting sulfonylurea anti-diabetic drug. It is marketed as Amaryl by Sanofi-Aventis and GLIMY by Dr.Reddy's Labs...
(Amaryl) - gliclazideGliclazideGliclazide is an oral hypoglycemic and is classified as a sulfonylurea. It is marketed as Glizid, Glyloc and Reclide in India and Diamicron in Canada. In the Philippines, Servier markets it as Diamicron MR, like in most countries across the world. Many generic equivalents are also available e.g....
(Diamicron)
- glipizide
Meglitinides
MeglitinideMeglitinide
Meglitinides, aka "Glinides", are a class of drugs used treat diabetes type 2.They bind to an ATP-dependent K+ channel on the cell membrane of pancreatic beta cells in a similar manner to sulfonylureas but at a separate binding site. This inhibits a tonic, hyperpolarizing outflux of potassium,...
s help the pancreas produce insulin and are often called "short-acting secretagogues." They act on the same potassium channels as sulfonylureas, but at a different binding site. By closing the potassium channels of the pancreatic beta cells, they open the calcium channels, hence enhancing insulin secretion.
They are taken with or shortly before meals to boost the insulin response to each meal. If a meal is skipped, the medication is also skipped.
Typical reductions in glycated hemoglobin (A1C) values are 0.5–1.0%.
- repaglinideRepaglinideRepaglinide is for the treatment of type II diabetes. It is supplied by Novo Nordisk...
(Prandin) - nateglinideNateglinideNateglinide is a drug for the treatment of type 2 diabetes. Nateglinide was developed by Ajinomoto, a Japanese company and sold by the Swiss pharmaceutical company Novartis....
(Starlix)
Adverse reactions include weight gain and hypoglycemia.
Alpha-glucosidase inhibitors
Alpha-glucosidase inhibitorAlpha-glucosidase inhibitor
Alpha-glucosidase inhibitors are oral anti-diabetic drugs used for diabetes mellitus type 2 that work by preventing the digestion of carbohydrates . Carbohydrates are normally converted into simple sugars , which can be absorbed through the intestine...
s are "diabetes pills" but not technically hypoglycemic agents because they do not have a direct effect on insulin secretion or sensitivity. These agents slow the digestion of starch in the small intestine, so that glucose from the starch of a meal enters the bloodstream more slowly, and can be matched more effectively by an impaired insulin response or sensitivity. These agents are effective by themselves only in the earliest stages of impaired glucose tolerance
Impaired glucose tolerance
Impaired glucose tolerance is a pre-diabetic state of dysglycemia that is associated with insulin resistance and increased risk of cardiovascular pathology. IGT may precede type 2 diabetes mellitus by many years...
, but can be helpful in combination with other agents in type 2 diabetes.
Typical reductions in glycated hemoglobin (A1C) values are 0.5–1.0%.
- miglitol (Glyset)
- acarboseAcarboseAcarbose is an anti-diabetic drug used to treat type 2 diabetes mellitus and, in some countries, prediabetes. It is a generic sold in Europe and China as Glucobay , in North America as Precose , and in Canada as Prandase...
(Precose/Glucobay)
These medications are rarely used in the United States because of the severity of their side effects (flatulence and bloating). They are more commonly prescribed in Europe. They do have the potential to cause weight loss by lowering the amount of sugar metabolized.
Research has shown the culinary mushroom maitake (Grifola frondosa
Grifola frondosa
Grifola frondosa is a polypore mushroom that grows in clusters at the base of trees, particularly oaks. The mushroom is commonly known among English speakers as Hen-of-the-Woods, Ram's Head and Sheep's Head...
) has a hypoglycemic
Blood sugar
The blood sugar concentration or blood glucose level is the amount of glucose present in the blood of a human or animal. Normally in mammals, the body maintains the blood glucose level at a reference range between about 3.6 and 5.8 mM , or 64.8 and 104.4 mg/dL...
effect, possibly due to the mushroom acting as a natural alpha glucosidase inhibitor.
Peptide analogs
Injectable Incretin mimetics
IncretinIncretin
Incretins are a group of gastrointestinal hormones that cause an increase in the amount of insulin released from the beta cells of the islets of Langerhans after eating, even before blood glucose levels become elevated. They also slow the rate of absorption of nutrients into the blood stream by...
s are insulin secretagogue
Secretagogue
A secretagogue is a substance that causes another substance to be secreted. One example is gastrin,, which stimulates the H/K ATPase in the parietal cells...
s. The two main candidate molecules that fulfill criteria for being an incretin are glucagon-like peptide-1
Glucagon-like peptide-1
Glucagon-like peptide-1 is derived from the transcription product of the proglucagon gene. The major source of GLP-1 in the body is the intestinal L cell that secretes GLP-1 as a gut hormone. The biologically active forms of GLP-1 are: GLP-1- and GLP-1-NH2...
(GLP-1) and gastric inhibitory peptide (glucose-dependent insulinotropic peptide, GIP). Both GLP-1 and GIP are rapidly inactivated by the enzyme dipeptidyl peptidase-4
Dipeptidyl peptidase-4
Dipeptidyl peptidase-4 , also known as adenosine deaminase complexing protein 2 or CD26 is a protein that, in humans, is encoded by the DPP4 gene.-Function:...
(DPP-4).
Injectable Glucagon-like peptide analogs and agonists
Glucagon-like peptide (GLP) agonists bind to a membrane GLP receptor. As a consequence, insulin release from the pancreatic beta cells is increased. Endogenous GLP has a half life of only a few minutes, thus an analogue of GLP would not be practical.- ExenatideExenatideExenatide is a medication approved in April 2005 for the treatment of diabetes mellitus type 2. It belongs to the group of incretin mimetics and is manufactured by Amylin Pharmaceuticals and Eli Lilly and Company....
(also Exendin-4, marketed as Byetta) is the first GLP-1Glucagon-like peptide-1Glucagon-like peptide-1 is derived from the transcription product of the proglucagon gene. The major source of GLP-1 in the body is the intestinal L cell that secretes GLP-1 as a gut hormone. The biologically active forms of GLP-1 are: GLP-1- and GLP-1-NH2...
agonist approved for the treatment of type 2 diabetes. Exenatide is not an analogue of GLP, but rather a GLP agonist. Exenatide has only 53% homology with GLP, which increases its resistance to degradation by DPP-4 and extends its half-life. Typical reductions in A1C values are 0.5–1.0%. - LiraglutideLiraglutideLiraglutide , marketed under the brand name Victoza, is a long-acting glucagon-like peptide-1 analog that has been developed by Novo Nordisk for the treatment of type 2 diabetes. The product was approved by the European Medicines Agency on July 3, 2009, and by the U.S...
, a once daily human analogue (97% homology), has been developed by Novo NordiskNovo NordiskNovo Nordisk manufactures and markets pharmaceutical products and services. Created in 1989 through a merger of two Danish companies dating back to the 1920s, it has become one of the world's leading companies in diabetes care, where Novo Nordisk pursues research into pulmonary delivery systems;...
under the brand name Victoza. The product was approved by the European Medicines AgencyEuropean Medicines AgencyThe European Medicines Agency is a European agency for the evaluation of medicinal products. From 1995 to 2004, the European Medicines Agency was known as European Agency for the Evaluation of Medicinal Products.Roughly parallel to the U.S...
(EMEA) on July 3, 2009, and by the U.S. Food and Drug Administration (FDA) on January 25, 2010. - TaspoglutideTaspoglutideTaspoglutide is a pharmaceutical drug. It is a glucagon-like peptide-1 analog, under investigation for treatment of type 2 diabetes being codeveloped by Ipsen and Roche.Two phase II trials reported it was effective and well tolerated....
is presently in Phase III clinical trials with Hoffman-La Roche.
These agents may also cause a decrease in gastric motility, responsible for the common side effect of nausea, and is probably the mechanism by which weight loss occurs.
Injectable peptide analogs
GLP-1 analogs resulted in weight loss and had more gastrointestinal side effects, while DPP-4 inhibitors were generally weight neutral and increased risk for infection and headache, but both classes appear to present an alternative to other antidiabetic drugs. However, weight gain and/or hypoglycaemia have been observed when DPP-4 inhibitors were used with sulfonylureas; effect on long-term health and morbidity rates are still unknown.Dipeptidyl peptidase-4 (DPP-4) inhibitors
Dipeptidyl peptidase-4 inhibitors
Inhibitors of dipeptidyl peptidase 4, also DPP-4 inhibitors or gliptins, are a class of oral hypoglycemics that block DPP-4. They can be used to treat diabetes mellitus type 2....
increase blood concentration of the incretin
Incretin
Incretins are a group of gastrointestinal hormones that cause an increase in the amount of insulin released from the beta cells of the islets of Langerhans after eating, even before blood glucose levels become elevated. They also slow the rate of absorption of nutrients into the blood stream by...
GLP-1 by inhibiting its degradation by dipeptidyl peptidase-4
Dipeptidyl peptidase-4
Dipeptidyl peptidase-4 , also known as adenosine deaminase complexing protein 2 or CD26 is a protein that, in humans, is encoded by the DPP4 gene.-Function:...
.
Examples are:
- vildagliptinVildagliptinVildagliptin is an oral anti-hyperglycemic agent of the new dipeptidyl peptidase-4 inhibitor class of drugs...
(Galvus) EU Approved 2008 - sitagliptinSitagliptinSitagliptin is an oral antihyperglycemic of the dipeptidyl peptidase-4 inhibitor class. It was developed, and is marketed, by Merck & Co...
(Januvia) FDA approved Oct 2006 - saxagliptinSaxagliptinSaxagliptin , previously identified as BMS-477118, is a new oral hypoglycemic of the new dipeptidyl peptidase-4 inhibitor class of drugs. Early development was solely by Bristol-Myers Squibb; in 2007 AstraZeneca joined with Bristol-Myers Squibb to co-develop the final compound and collaborate on...
(Onglyza) FDA Approved July 2009 - linagliptinLinagliptinLinagliptin is a DPP-4 inhibitor developed by Boehringer Ingelheim for treatment of type II diabetes....
(Tradjenta) FDA Approved May 2, 2011
DPP-4 inhibitors lowered hemoglobin A1C values by 0.74%, comparable to other antidiabetic drugs.
In one RCT comprising 206 patients aged 65 or older (mean baseline HgbA1c of 7.8%) receiving either 50 or 100 mg/d of Sitagliptin
Sitagliptin
Sitagliptin is an oral antihyperglycemic of the dipeptidyl peptidase-4 inhibitor class. It was developed, and is marketed, by Merck & Co...
was shown to reduce HbA1c by 0.7% (combined result of both doses). A combined result of 5 RCTs enlisting a total of 279 patients aged 65 or older (mean baseline HbA1c of 8%) receiving 5 mg/d of Saxagliptin
Saxagliptin
Saxagliptin , previously identified as BMS-477118, is a new oral hypoglycemic of the new dipeptidyl peptidase-4 inhibitor class of drugs. Early development was solely by Bristol-Myers Squibb; in 2007 AstraZeneca joined with Bristol-Myers Squibb to co-develop the final compound and collaborate on...
was shown to reduce HbA1c by 0.73%. A combined result of 5 RCTs enlisting a total of 238 patients aged 65 or older (mean baseline HbA1c of 8.6%) receiving 100 mg/d of Vildagliptin
Vildagliptin
Vildagliptin is an oral anti-hyperglycemic agent of the new dipeptidyl peptidase-4 inhibitor class of drugs...
was shown to reduce HbA1c by 1.2%. Another set of 6 combined RCTs involving Alogliptin
Alogliptin
Alogliptin is an investigational anti-diabetic drug in the DPP-4 inhibitor class, being developed by Takeda Pharmaceutical Company. In January 2008, Takeda submitted a New Drug Application for alogliptin to the U.S. Food and Drug Administration, after positive results from Phase III clinical trials...
(not yet approved, might be released in 2012) was shown to reduce HbA1c by 0.73% in 455 patients aged 65 or older who received 12.5 or 25 mg/d of the medication.
Injectable Amylin analogues
AmylinAmylin
Amylin, or Islet Amyloid Polypeptide , is a 37-residue peptide hormone secreted by pancreatic β-cells at the same time as insulin .-Clinical significance:...
agonist analogues slow gastric emptying and suppress glucagon
Glucagon
Glucagon, a hormone secreted by the pancreas, raises blood glucose levels. Its effect is opposite that of insulin, which lowers blood glucose levels. The pancreas releases glucagon when blood sugar levels fall too low. Glucagon causes the liver to convert stored glycogen into glucose, which is...
. They have all the incretins actions except stimulation of insulin secretion. , pramlintide
Pramlintide
Pramlintide acetate is a relatively new adjunct for diabetes , developed by Amylin Pharmaceuticals.-Pharmacology:...
is the only clinically available amylin analogue. Like insulin, it is administered by subcutaneous injection
Subcutaneous injection
A subcutaneous injection is administered as a bolus into the subcutis, the layer of skin directly below the dermis and epidermis, collectively referred to as the...
. The most frequent and severe adverse effect of pramlintide is nausea
Nausea
Nausea , is a sensation of unease and discomfort in the upper stomach with an involuntary urge to vomit. It often, but not always, precedes vomiting...
, which occurs mostly at the beginning of treatment and gradually reduces. Typical reductions in A1C values are 0.5–1.0%.
Comparison
The following table compares some common anti-diabetic agents, generalizing classes although there may be substantial variation in individual drugs of each class:| Agent | Mechanism | Site of action | Main advantages | Main side effect Side effect In medicine, a side effect is an effect, whether therapeutic or adverse, that is secondary to the one intended; although the term is predominantly employed to describe adverse effects, it can also apply to beneficial, but unintended, consequences of the use of a drug.Occasionally, drugs are... s |
|---|---|---|---|---|
| Sulfonylurea Sulfonylurea Sulfonylurea derivatives are a class of antidiabetic drugs that are used in the management of diabetes mellitus type 2. They act by increasing insulin release from the beta cells in the pancreas.-First generation:* Carbutamide... s |
Stimulating insulin production by inhibiting the KATP channel | Pancreatic beta cell Beta cell Beta cells are a type of cell in the pancreas located in the so-called islets of Langerhans. They make up 65-80% of the cells in the islets.-Function:... s |
|
Hypoglycemia Hypoglycemia or hypoglycæmia is the medical term for a state produced by a lower than normal level of blood glucose. The term literally means "under-sweet blood"... Weight gain Weight gain is an increase in body weight. This can be either an increase in muscle mass, fat deposits, or excess fluids such as water.-Description:... |
| Metformin Metformin Metformin is an oral antidiabetic drug in the biguanide class. It is the first-line drug of choice for the treatment of type 2 diabetes, in particular, in overweight and obese people and those with normal kidney function. Its use in gestational diabetes has been limited by safety concerns... |
Decreases insulin resistance Insulin resistance Insulin resistance is a physiological condition where the natural hormone insulin becomes less effective at lowering blood sugars. The resulting increase in blood glucose may raise levels outside the normal range and cause adverse health effects, depending on dietary conditions. Certain cell types... |
Liver |
|
Lactic acidosis Lactic acidosis is a physiological condition characterized by low pH in body tissues and blood accompanied by the buildup of lactate especially D-lactate, and is considered a distinct form of metabolic acidosis. The condition typically occurs when cells receive too little oxygen , for example... |
| Acarbose Acarbose Acarbose is an anti-diabetic drug used to treat type 2 diabetes mellitus and, in some countries, prediabetes. It is a generic sold in Europe and China as Glucobay , in North America as Precose , and in Canada as Prandase... |
Reduces intestinal glucose absorption | GI tract Gastrointestinal tract The human gastrointestinal tract refers to the stomach and intestine, and sometimes to all the structures from the mouth to the anus. .... |
|
Flatulence Flatulence is the expulsion through the rectum of a mixture of gases that are byproducts of the digestion process of mammals and other animals. The medical term for the mixture of gases is flatus, informally known as a fart, or simply gas... |
| Thiazolidinediones | Reduce insulin resistance by activating PPAR-γ Peroxisome proliferator-activated receptor gamma Peroxisome proliferator-activated receptor gamma , also known as the glitazone receptor, or NR1C3 is a type II nuclear receptor that in humans is encoded by the PPARG gene.Two isoforms of PPARG are detected in the human and in the mouse: PPAR-γ1 and... |
Fat, muscle | Hepatoxicity |
Most anti-diabetic agents are contraindicated in pregnancy, in which insulin is preferred.
Alternative medicine
A number of medicinal plants have been studied for the treatment of diabetes however there is insufficient evidence to determine their effectiveness. CinnamonCinnamon
Cinnamon is a spice obtained from the inner bark of several trees from the genus Cinnamomum that is used in both sweet and savoury foods...
has blood sugar lowering properties however whether or not it is useful for treating diabetes is unknown. While chromium supplements have no beneficial effect on healthy people, there might be an improvement in glucose metabolism in those with diabetics, although the evidence for this effect remains weak. Vanadyl sulfate, a salt of vanadium
Vanadium
Vanadium is a chemical element with the symbol V and atomic number 23. It is a hard, silvery gray, ductile and malleable transition metal. The formation of an oxide layer stabilizes the metal against oxidation. The element is found only in chemically combined form in nature...
, is still in preliminary studies. There is tentative research that thiamine
Thiamine
Thiamine or thiamin or vitamin B1 , named as the "thio-vitamine" is a water-soluble vitamin of the B complex. First named aneurin for the detrimental neurological effects if not present in the diet, it was eventually assigned the generic descriptor name vitamin B1. Its phosphate derivatives are...
may prevent some diabetic complications however more research is needed.

