
Islet cell transplantation
Encyclopedia
Islet transplantation is the transplantation
of isolated islets from a donor pancreas
and into another person. It is an experimental treatment for type 1 diabetes mellitus. Once transplanted, the islets begin to produce insulin
, actively regulating the level of glucose
in the blood
.
Islets are usually infused into the patient's liver
,. If the cells are not from a genetically identical donor the patients body will recognize them as foreign and the immune system
will begin to attack them as with any transplant rejection
. To prevent this immunosupressant drugs are used. Recent studies have shown that islet transplantation has progressed to the point that 58% of the patients in one study were insulin independent one year after the operation.
In the period from 1999 to 2004, 471 patients with type 1 diabetes have received islet transplants at 43 institutions worldwide.
and in vivo
islet experiments. Subsequent studies showed that transplanted islets could reverse diabetes in both rodent
s and non-human primate
s. In a summary of the 1977 Workshop on Pancreatic Islet Cell Transplantation in Diabetes, Lacy commented on the feasibility of “islet cell transplantation as a therapeutic approach [for] the possible prevention of the complications of diabetes in man”. Improvements in isolation techniques and immunosuppressive regimens ushered in the first human islet transplantation clinical trials in the mid-1980s. The first successful trial of human islet allotransplantation resulting in long-term reversal of diabetes was performed at the University of Pittsburgh in 1990. Yet despite continued procedural improvements, only about 10% of islet recipients in the late 1990s achieved euglycemia (normal blood glucose). In 2000, Dr. James Shapiro and colleagues published a report describing seven consecutive patients who achieved euglycemia following islet transplantation using a steroid-free protocol and large numbers of donor islets, since referred to as the Edmonton protocol
. This protocol has been adapted by islet transplant centers around the world and has greatly increased islet transplant success.
level removing the need for insulin injections. For an average-size person (70 kg), a typical transplant requires about one million islets, isolated from two donor pancreases. Because good control of blood glucose can slow or prevent the progression of complications associated with diabetes, such as nerve or eye damage
, a successful transplant may reduce the risk of these complications. But a transplant recipient will need to take immunosuppressive drugs that stop the immune system from rejecting the transplanted islets.
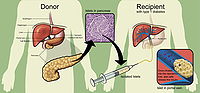 Researchers use a mixture of highly purified enzymes (Collagenase) to isolate islets from the pancreas of a deceased donor. Collagenase solution is injected into the pancreatic duct
Researchers use a mixture of highly purified enzymes (Collagenase) to isolate islets from the pancreas of a deceased donor. Collagenase solution is injected into the pancreatic duct
which runs through the head, body and tail of the pancreas. Delivered this way, the enzyme solution causes distension of the pancreas, which is subsequently cut into small chunks and transferred into so-called Ricordi's chamber, where digestion takes place until the islets are liberated and removed from the solution. Isolated islets are then separated from the exocrine tissue
and debris in a process called purification.
During the transplant, a radiologist uses ultrasound
and radiography
to guide placement of a catheter through the upper abdomen and into the portal vein of the liver. The islets are then infused through the catheter into the liver. The patient will receive a local anesthetic
. If a patient cannot tolerate local anesthesia, the surgeon may use general anesthesia and do the transplant through a small incision. Possible risks of the procedure include bleeding or blood clots.
It takes time for the islets to attach to new blood vessels and begin releasing insulin. The doctor will order many tests to check blood glucose levels after the transplant, and insulin may be needed until control is achieved.
uses a combination of immunosuppressive drug
s, including daclizumab
(Zenapax), sirolimus
(Rapamune) and tacrolimus
(Prograf). Daclizumab is given intravenously right after the transplant and then discontinued. Sirolimus and tacrolimus, the two main drugs that keep the immune system from destroying the transplanted islets, must be taken for life.
, anemia
, weight loss
, hypertension
, hyperlipidemia
, diarrhea
and fatigue
. Perhaps of greatest concern to the patient and physician is the harmful effect of certain widely employed immunosuppressive agents on renal function
. For the patient with diabetes, renal function is a crucial factor in determining long-term outcome, and calcineurin inhibitors (tacrolimus
and ciclosporin
) are significantly nephrotoxic
. Thus, while some patients with a pancreas transplant tolerate the immunosuppressive agents well, and for such patients diabetic nephropathy can gradually improve, in other patients the net effect (decreased risk due to the improved blood glucose control, increased risk from the immunosuppressive agents) may worsen kidney function. Indeed, Ojo et al. have published an analysis indicating that among patients receiving other-than-kidney allografts, 7%–21% end up with renal failure as a result of the transplant and/or subsequent immunosuppression.
Seen another way, patients with heart
, liver
, lung
, or kidney failure have a dismal prognosis for survival, so the toxicity associated with immunosuppression is warranted (the benefits of graft survival outweigh the risks associated with the medications). But for the subset of patients with diabetes and preserved kidney function, even those with long-standing and difficult-to-control disease, the prognosis for survival is comparatively much better. In addition to the immunosuppressive toxicities, other risks are associated with the islet transplant procedure itself, including intra-abdominal hemorrhage following the transplant, and portal vein thrombosis
. The fact that there is already a good alternative to islet transplantation (i.e. the modern intensive insulin regimen) forces us to regard any newer, riskier interventions with a critical eye.
Like all transplantation therapies, islet transplantation is also handicapped by the limited donor pool. The numbers are striking; at least 1 million Americans have type 1 diabetes mellitus, and only a few thousand donor pancreata are available each year. To circumvent this organ shortage problem, researchers continue to look for ways to "grow" islets—or at least cells capable of physiologically regulated insulin secretion—in vitro, but currently only islets from cadaveric donors can be used to restore euglycemia. Further exacerbating the problem (and unlike kidney, liver, and heart transplants, where only one donor is needed for each recipient) most islet transplant patients require islets from two or more donors to achieve euglycemia. Lastly, the current methods for islet isolation need improvement, since only about half of attempted isolations produce transplant-ready islets.
While islet transplantation research has made important progress and the success stories are encouraging, the long-term safety and efficacy of the procedure remain unclear. Other concerns relating to the field include questions about the impact of having insulin-producing foreign cells within the hepatic parenchyma
, the long-term consequences of elevated portal pressures resulting from the islet infusion, and the fact that islet recipients can be sensitized against donor tissue types, making it more difficult to find a suitable donor should another life-saving transplant be required in the future. Also, very few islet transplant recipients have remained euglycemic without the use of any exogenous insulin beyond four years post-transplant. Thus, while most islet recipients achieve better glycemia control and suffer less serious hypoglycemia, islet transplantation continues to fall short of the definitive diabetes cure.
y agents offer the greatest hope of revolutionizing the field. New drug regimens capable of inducing tolerance to the transplanted islets would allow recipients to maintain their grafts without general immunosuppression and its associated toxicities. While many targets are currently under investigation, none are ready for clinical use.
Organ transplant
Organ transplantation is the moving of an organ from one body to another or from a donor site on the patient's own body, for the purpose of replacing the recipient's damaged or absent organ. The emerging field of regenerative medicine is allowing scientists and engineers to create organs to be...
of isolated islets from a donor pancreas
Pancreas
The pancreas is a gland organ in the digestive and endocrine system of vertebrates. It is both an endocrine gland producing several important hormones, including insulin, glucagon, and somatostatin, as well as a digestive organ, secreting pancreatic juice containing digestive enzymes that assist...
and into another person. It is an experimental treatment for type 1 diabetes mellitus. Once transplanted, the islets begin to produce insulin
Insulin
Insulin is a hormone central to regulating carbohydrate and fat metabolism in the body. Insulin causes cells in the liver, muscle, and fat tissue to take up glucose from the blood, storing it as glycogen in the liver and muscle....
, actively regulating the level of glucose
Glucose
Glucose is a simple sugar and an important carbohydrate in biology. Cells use it as the primary source of energy and a metabolic intermediate...
in the blood
Blood
Blood is a specialized bodily fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells....
.
Islets are usually infused into the patient's liver
Liver
The liver is a vital organ present in vertebrates and some other animals. It has a wide range of functions, including detoxification, protein synthesis, and production of biochemicals necessary for digestion...
,. If the cells are not from a genetically identical donor the patients body will recognize them as foreign and the immune system
Immune system
An immune system is a system of biological structures and processes within an organism that protects against disease by identifying and killing pathogens and tumor cells. It detects a wide variety of agents, from viruses to parasitic worms, and needs to distinguish them from the organism's own...
will begin to attack them as with any transplant rejection
Transplant rejection
Transplant rejection occurs when transplanted tissue is rejected by the recipient's immune system, which destroys the transplanted tissue. Transplant rejection can be lessened by determining the molecular similitude between donor and recipient and by use of immunosuppressant drugs after...
. To prevent this immunosupressant drugs are used. Recent studies have shown that islet transplantation has progressed to the point that 58% of the patients in one study were insulin independent one year after the operation.
In the period from 1999 to 2004, 471 patients with type 1 diabetes have received islet transplants at 43 institutions worldwide.
History
The concept of islet transplantation is not new. Investigators as early as the English surgeon Charles Pybus (1882–1975) attempted to graft pancreatic tissue to cure diabetes. Most, however, credit the recent era of islet transplantation research to Paul Lacy's studies dating back more than three decades. In 1967, Lacy's group described a novel collagenase-based method (later modified by Dr. Camillo Ricordi, then working with Dr. Lacy) to isolate islets, paving the way for future in vitroIn vitro
In vitro refers to studies in experimental biology that are conducted using components of an organism that have been isolated from their usual biological context in order to permit a more detailed or more convenient analysis than can be done with whole organisms. Colloquially, these experiments...
and in vivo
In vivo
In vivo is experimentation using a whole, living organism as opposed to a partial or dead organism, or an in vitro controlled environment. Animal testing and clinical trials are two forms of in vivo research...
islet experiments. Subsequent studies showed that transplanted islets could reverse diabetes in both rodent
Rodent
Rodentia is an order of mammals also known as rodents, characterised by two continuously growing incisors in the upper and lower jaws which must be kept short by gnawing....
s and non-human primate
Primate
A primate is a mammal of the order Primates , which contains prosimians and simians. Primates arose from ancestors that lived in the trees of tropical forests; many primate characteristics represent adaptations to life in this challenging three-dimensional environment...
s. In a summary of the 1977 Workshop on Pancreatic Islet Cell Transplantation in Diabetes, Lacy commented on the feasibility of “islet cell transplantation as a therapeutic approach [for] the possible prevention of the complications of diabetes in man”. Improvements in isolation techniques and immunosuppressive regimens ushered in the first human islet transplantation clinical trials in the mid-1980s. The first successful trial of human islet allotransplantation resulting in long-term reversal of diabetes was performed at the University of Pittsburgh in 1990. Yet despite continued procedural improvements, only about 10% of islet recipients in the late 1990s achieved euglycemia (normal blood glucose). In 2000, Dr. James Shapiro and colleagues published a report describing seven consecutive patients who achieved euglycemia following islet transplantation using a steroid-free protocol and large numbers of donor islets, since referred to as the Edmonton protocol
Edmonton protocol
The Edmonton Protocol is a method of implantation of pancreatic islets for the treatment of type 1 diabetes mellitus, specifically "brittle" type 1 diabetics prone to hypoglycemic unawareness...
. This protocol has been adapted by islet transplant centers around the world and has greatly increased islet transplant success.
Goals
The goal of islet transplantation is to infuse enough islets to control the blood glucoseBlood sugar
The blood sugar concentration or blood glucose level is the amount of glucose present in the blood of a human or animal. Normally in mammals, the body maintains the blood glucose level at a reference range between about 3.6 and 5.8 mM , or 64.8 and 104.4 mg/dL...
level removing the need for insulin injections. For an average-size person (70 kg), a typical transplant requires about one million islets, isolated from two donor pancreases. Because good control of blood glucose can slow or prevent the progression of complications associated with diabetes, such as nerve or eye damage
Retinopathy
Retinopathy is a general term that refers to some form of non-inflammatory damage to the retina of the eye. Frequently, retinopathy is an ocular manifestation of systemic disease.-Pathophysiology:Causes of retinopathy are varied:...
, a successful transplant may reduce the risk of these complications. But a transplant recipient will need to take immunosuppressive drugs that stop the immune system from rejecting the transplanted islets.
Procedure
Pancreatic duct
The pancreatic duct, or duct of Wirsung , is a duct joining the pancreas to the common bile duct to supply pancreatic juices which aid in digestion provided by the "exocrine pancreas"...
which runs through the head, body and tail of the pancreas. Delivered this way, the enzyme solution causes distension of the pancreas, which is subsequently cut into small chunks and transferred into so-called Ricordi's chamber, where digestion takes place until the islets are liberated and removed from the solution. Isolated islets are then separated from the exocrine tissue
Exocrine pancreas
The exocrine pancreas has ducts that are arranged in clusters called acini . Pancreatic secretions are secreted into the lumen of the acinus, and then accumulate in intralobular ducts that drain to the main pancreatic duct, which drains directly into the duodenum.Control of the exocrine function of...
and debris in a process called purification.
During the transplant, a radiologist uses ultrasound
Medical ultrasonography
Diagnostic sonography is an ultrasound-based diagnostic imaging technique used for visualizing subcutaneous body structures including tendons, muscles, joints, vessels and internal organs for possible pathology or lesions...
and radiography
Radiography
Radiography is the use of X-rays to view a non-uniformly composed material such as the human body. By using the physical properties of the ray an image can be developed which displays areas of different density and composition....
to guide placement of a catheter through the upper abdomen and into the portal vein of the liver. The islets are then infused through the catheter into the liver. The patient will receive a local anesthetic
Local anesthetic
A local anesthetic is a drug that causes reversible local anesthesia, generally for the aim of having local analgesic effect, that is, inducing absence of pain sensation, although other local senses are often affected as well...
. If a patient cannot tolerate local anesthesia, the surgeon may use general anesthesia and do the transplant through a small incision. Possible risks of the procedure include bleeding or blood clots.
It takes time for the islets to attach to new blood vessels and begin releasing insulin. The doctor will order many tests to check blood glucose levels after the transplant, and insulin may be needed until control is achieved.
Immunosuppression
The Edmonton protocolEdmonton protocol
The Edmonton Protocol is a method of implantation of pancreatic islets for the treatment of type 1 diabetes mellitus, specifically "brittle" type 1 diabetics prone to hypoglycemic unawareness...
uses a combination of immunosuppressive drug
Immunosuppressive drug
Immunosuppressive drugs or immunosuppressive agents are drugs that inhibit or prevent activity of the immune system. They are used in immunosuppressive therapy to:...
s, including daclizumab
Daclizumab
Daclizumab is a therapeutic humanized monoclonal antibody to the alpha subunit of the IL-2 receptor of T cells. It is used to prevent rejection in organ transplantation, especially in kidney transplants....
(Zenapax), sirolimus
Sirolimus
Sirolimus , also known as rapamycin, is an immunosuppressant drug used to prevent rejection in organ transplantation; it is especially useful in kidney transplants. A macrolide, sirolimus was first discovered as a product of the bacterium Streptomyces hygroscopicus in a soil sample from Easter...
(Rapamune) and tacrolimus
Tacrolimus
Tacrolimus is an immunosuppressive drug that is mainly used after allogeneic organ transplant to reduce the activity of the patient's immune system and so lower the risk of organ rejection...
(Prograf). Daclizumab is given intravenously right after the transplant and then discontinued. Sirolimus and tacrolimus, the two main drugs that keep the immune system from destroying the transplanted islets, must be taken for life.
Limitations
While significant progress has been made in the islet transplantation field, many obstacles remain that currently preclude its widespread application. Two of the most important limitations are the currently inadequate means for preventing islet rejection, and the limited supply of islets for transplantation. Current immunosuppressive regimens are capable of preventing islet failure for months to years, but the agents used in these treatments are expensive and may increase the risk for specific malignancies and opportunistic infections. In addition, and somewhat ironically, the most commonly used agents (like calcineurin inhibitors and rapamycin) are also known to impair normal islet function and/or insulin action. Further, like all medications, the agents have other associated toxicities, with side effects such as oral ulcers, peripheral edemaPeripheral edema
Peripheral edema is the swelling of tissues, usually in the lower limbs, due to the accumulation of fluids.The condition is commonly associated with aging, but can be caused by many other conditions, including congestive heart failure, trauma, alcoholism, altitude sickness, pregnancy,...
, anemia
Anemia
Anemia is a decrease in number of red blood cells or less than the normal quantity of hemoglobin in the blood. However, it can include decreased oxygen-binding ability of each hemoglobin molecule due to deformity or lack in numerical development as in some other types of hemoglobin...
, weight loss
Weight loss
Weight loss, in the context of medicine, health or physical fitness, is a reduction of the total body mass, due to a mean loss of fluid, body fat or adipose tissue and/or lean mass, namely bone mineral deposits, muscle, tendon and other connective tissue...
, hypertension
Hypertension
Hypertension or high blood pressure is a cardiac chronic medical condition in which the systemic arterial blood pressure is elevated. What that means is that the heart is having to work harder than it should to pump the blood around the body. Blood pressure involves two measurements, systolic and...
, hyperlipidemia
Hyperlipidemia
Hyperlipidemia, hyperlipoproteinemia, or hyperlipidaemia is the condition of abnormally elevated levels of any or all lipids and/or lipoproteins in the blood...
, diarrhea
Diarrhea
Diarrhea , also spelled diarrhoea, is the condition of having three or more loose or liquid bowel movements per day. It is a common cause of death in developing countries and the second most common cause of infant deaths worldwide. The loss of fluids through diarrhea can cause dehydration and...
and fatigue
Fatigue (physical)
Fatigue is a state of awareness describing a range of afflictions, usually associated with physical and/or mental weakness, though varying from a general state of lethargy to a specific work-induced burning sensation within one's muscles...
. Perhaps of greatest concern to the patient and physician is the harmful effect of certain widely employed immunosuppressive agents on renal function
Renal function
Renal function, in nephrology, is an indication of the state of the kidney and its role in renal physiology. Glomerular filtration rate describes the flow rate of filtered fluid through the kidney...
. For the patient with diabetes, renal function is a crucial factor in determining long-term outcome, and calcineurin inhibitors (tacrolimus
Tacrolimus
Tacrolimus is an immunosuppressive drug that is mainly used after allogeneic organ transplant to reduce the activity of the patient's immune system and so lower the risk of organ rejection...
and ciclosporin
Ciclosporin
Ciclosporin , cyclosporine , cyclosporin , or cyclosporin A is an immunosuppressant drug widely used in post-allogeneic organ transplant to reduce the activity of the immune system, and therefore the risk of organ rejection...
) are significantly nephrotoxic
Nephrotoxicity
Nephrotoxicity is a poisonous effect of some substances, both toxic chemicals and medication, on the kidneys. There are various forms of toxicity. Nephrotoxicity should not be confused with the fact that some medications have a predominantly renal excretion and need their dose adjusted for the...
. Thus, while some patients with a pancreas transplant tolerate the immunosuppressive agents well, and for such patients diabetic nephropathy can gradually improve, in other patients the net effect (decreased risk due to the improved blood glucose control, increased risk from the immunosuppressive agents) may worsen kidney function. Indeed, Ojo et al. have published an analysis indicating that among patients receiving other-than-kidney allografts, 7%–21% end up with renal failure as a result of the transplant and/or subsequent immunosuppression.
Seen another way, patients with heart
Congestive heart failure
Heart failure often called congestive heart failure is generally defined as the inability of the heart to supply sufficient blood flow to meet the needs of the body. Heart failure can cause a number of symptoms including shortness of breath, leg swelling, and exercise intolerance. The condition...
, liver
Liver failure
Acute liver failure is the appearance of severe complications rapidly after the first signs of liver disease , and indicates that the liver has sustained severe damage . The complications are hepatic encephalopathy and impaired protein synthesis...
, lung
Respiratory failure
The term respiratory failure, in medicine, is used to describe inadequate gas exchange by the respiratory system, with the result that arterial oxygen and/or carbon dioxide levels cannot be maintained within their normal ranges. A drop in blood oxygenation is known as hypoxemia; a rise in arterial...
, or kidney failure have a dismal prognosis for survival, so the toxicity associated with immunosuppression is warranted (the benefits of graft survival outweigh the risks associated with the medications). But for the subset of patients with diabetes and preserved kidney function, even those with long-standing and difficult-to-control disease, the prognosis for survival is comparatively much better. In addition to the immunosuppressive toxicities, other risks are associated with the islet transplant procedure itself, including intra-abdominal hemorrhage following the transplant, and portal vein thrombosis
Portal vein thrombosis
Portal vein thrombosis is a form of venous thrombosis affecting the hepatic portal vein, which can lead to portal hypertension and reduction in the blood supply to the liver.-Causes:...
. The fact that there is already a good alternative to islet transplantation (i.e. the modern intensive insulin regimen) forces us to regard any newer, riskier interventions with a critical eye.
Like all transplantation therapies, islet transplantation is also handicapped by the limited donor pool. The numbers are striking; at least 1 million Americans have type 1 diabetes mellitus, and only a few thousand donor pancreata are available each year. To circumvent this organ shortage problem, researchers continue to look for ways to "grow" islets—or at least cells capable of physiologically regulated insulin secretion—in vitro, but currently only islets from cadaveric donors can be used to restore euglycemia. Further exacerbating the problem (and unlike kidney, liver, and heart transplants, where only one donor is needed for each recipient) most islet transplant patients require islets from two or more donors to achieve euglycemia. Lastly, the current methods for islet isolation need improvement, since only about half of attempted isolations produce transplant-ready islets.
While islet transplantation research has made important progress and the success stories are encouraging, the long-term safety and efficacy of the procedure remain unclear. Other concerns relating to the field include questions about the impact of having insulin-producing foreign cells within the hepatic parenchyma
Parenchyma
Parenchyma is a term used to describe a bulk of a substance. It is used in different ways in animals and in plants.The term is New Latin, f. Greek παρέγχυμα - parenkhuma, "visceral flesh", f. παρεγχεῖν - parenkhein, "to pour in" f. para-, "beside" + en-, "in" + khein, "to pour"...
, the long-term consequences of elevated portal pressures resulting from the islet infusion, and the fact that islet recipients can be sensitized against donor tissue types, making it more difficult to find a suitable donor should another life-saving transplant be required in the future. Also, very few islet transplant recipients have remained euglycemic without the use of any exogenous insulin beyond four years post-transplant. Thus, while most islet recipients achieve better glycemia control and suffer less serious hypoglycemia, islet transplantation continues to fall short of the definitive diabetes cure.
Future
Just as early studies showed islet transplantation's promise, research must now overcome the hurdles revealed by the recent islet transplant experience. New immunomodulatorImmunomodulator
An immunomodulator, also known as an immunotherapy is a substance which has an effect on the immune system.- Immunosuppressants :Inhibits immune response in organ transplantation and autoimmune diseases.- Immunostimulants :...
y agents offer the greatest hope of revolutionizing the field. New drug regimens capable of inducing tolerance to the transplanted islets would allow recipients to maintain their grafts without general immunosuppression and its associated toxicities. While many targets are currently under investigation, none are ready for clinical use.
External links
- VIDEO: Update on Islet Transplantation at the University of Wisconsin Dr. Luis Fernandez, November 2007.
- Clinical Islet Transplant Program - University of Alberta
- Diabetes Research Institute http://www.drinet.org
- Miami Islet Recipients http://www.islets.fanspace.com
- Mayo Clinic: Islet cell transplant: Emerging treatment for type 1 diabetes
- Islet Cell Transplant Program - UW Health
- Immune Tolerance Network
- Uppsala University Hospital

