Clinical governance
Encyclopedia
Clinical governance is the term used to describe a systematic approach to maintaining and improving the quality of patient care within a health system. The term became widely used in health care following the Bristol heart scandal
in 1995, during which anaesthetist Dr Stephen Bolsin
exposed the high mortality rate for paediatric cardiac surgery at the Bristol Royal Infirmary. It was originally elaborated within the United Kingdom
National Health Service
(NHS), and its most widely cited formal definition describes it as:
This definition is intended to embody three key attributes: recognisably high standards of care, transparent responsibility and accountability for those standards, and a constant dynamic of improvement.
The concept has some parallels with the more widely known corporate governance
, in that it addresses those structures, systems and processes that assure the quality, accountability and proper management of an organisation's operation and delivery of service. However clinical governance applies only to health and social care organisations, and only those aspects of such organisations that relate to the delivery of care to patients and their carers; it is not concerned with the other business processes of the organisation except insofar as they affect the delivery of care. The concept of "integrated governance
" has emerged to refer jointly to the corporate governance and clinical governance duties of healthcare organisations.
Prior to 1999, the principal statutory responsibilities of UK NHS Trust Boards were to ensure proper financial management of the organisation and an acceptable level of patient safety. Trust Boards had no statutory duty to ensure a particular level of quality. Maintaining and improving the quality of care was understood to be the responsibility of the relevant clinical professions. As of 1999, Trust Boards assumed a legal responsibility for quality of care that is equal in measure to their other statutory duties. Clinical governance is the mechanism by which that responsibility is discharged.
"Clinical governance" does not mandate any particular structure, system or process for maintaining and improving the quality of care, except that designated responsibility for clinical governance must exist at Trust Board level, and that each Trust must prepare an Annual Review of Clinical Governance to report on quality of care and its maintenance. Beyond that, the Trust and its various clinical departments are obliged to interpret the principle of clinical governance into locally appropriate structures, processes, roles and responsibilities.
"Clinical Governance" is also one of the most frequently-occurring phrases in buzzword bingo
.
 Clinical governance is composed of at least the following elements:
Clinical governance is composed of at least the following elements:
after qualification - too much of what is learned during training becomes quickly outdated. In NHS
Trusts, the continuing professional development of clinicians has been the responsibility of the Trust also been the professional duty of clinicians to remain up-to-date.
Trust employees, in primary care
clinical audit has only been encouraged, where audit time has had to compete with other priorities.
Techniques such as critical appraisal
of the literature, project management
and the development of guidelines, protocols
and implementation strategies are all tools for promoting the implementation of research practice.
Any organisation providing high quality care has to show that it is meeting the needs of the population it serves. Health needs assessment and understanding the problems and aspirations of the community requires the cooperation between NHS
organisations, public health departments, local authorities and community health councils.
The system of clinical governance brings together all the elements which seek to promote quality of care.
Risks to patients: compliance with statutory regulations can help to minimise risks to patients. In addition, patient risks can be minimised by ensuring that systems are regularly reviewed and questioned - for example, by critical event audit and learning from complaints. Medical ethical standards
are also a key factor in maintaining patient and public safety and well-being.
Risks to practitioners: ensuring that clinicians are immunised against infectious diseases, work in a safe environment and are helped to keep up-to-date are important parts of quality assurance.
Risks to the organisation: poor quality is a threat to any organisation. In addition to reducing risks to patients and practitioners, organisations need to reduce their own risks by ensuring high quality employment practice (including locum procedures and reviews of individual and team performance), a safe environment (including estates and privacy), and well designed policies on public involvement.
Patient records (demographic, Socioeconomic, Clinical information) proper collection, management and use of information within healthcare systems “will determine the system’s effectiveness in detecting health problems, defining priorities, identifying innovative solutions and allocating resources to improve health outcomes.
The system has found supporters outside of the UK. The not-for-profit UK hospital accreditation group the Trent Accreditation Scheme
base their system upon NHS clinical governance, and apply it to hospitals in Hong Kong
and Malta
.
Bristol heart scandal
The Bristol heart scandal occurred in England during the 1990s. At the Bristol Royal Infirmary, babies died at high rates after cardiac surgery. An inquiry found "staff shortages, a lack of leadership, [a] ... unit ... 'simply not up to the task' ... 'an old boy's culture' among doctors, a lax...
in 1995, during which anaesthetist Dr Stephen Bolsin
Stephen Bolsin
Stephen Nicholas Cluley Bolsin is a British anaesthetist who became famous as the whistleblower whose actions to prevent incompetent paediatric cardiac surgery at the Bristol Royal Infirmary lead to the implementation of clinical governance reforms in the United Kingdom.- Career background...
exposed the high mortality rate for paediatric cardiac surgery at the Bristol Royal Infirmary. It was originally elaborated within the United Kingdom
United Kingdom
The United Kingdom of Great Britain and Northern IrelandIn the United Kingdom and Dependencies, other languages have been officially recognised as legitimate autochthonous languages under the European Charter for Regional or Minority Languages...
National Health Service
National Health Service
The National Health Service is the shared name of three of the four publicly funded healthcare systems in the United Kingdom. They provide a comprehensive range of health services, the vast majority of which are free at the point of use to residents of the United Kingdom...
(NHS), and its most widely cited formal definition describes it as:
A framework through which NHS organisations are accountable for continually improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish.
This definition is intended to embody three key attributes: recognisably high standards of care, transparent responsibility and accountability for those standards, and a constant dynamic of improvement.
The concept has some parallels with the more widely known corporate governance
Corporate governance
Corporate governance is a number of processes, customs, policies, laws, and institutions which have impact on the way a company is controlled...
, in that it addresses those structures, systems and processes that assure the quality, accountability and proper management of an organisation's operation and delivery of service. However clinical governance applies only to health and social care organisations, and only those aspects of such organisations that relate to the delivery of care to patients and their carers; it is not concerned with the other business processes of the organisation except insofar as they affect the delivery of care. The concept of "integrated governance
Integrated governance
Integrated governance is the process of "systems, processes and behaviours by which NHS trusts providing services for the National Health Service in the United Kingdom lead, direct and control their functions in order to achieve organisational objectives, safety and quality of service, and in which...
" has emerged to refer jointly to the corporate governance and clinical governance duties of healthcare organisations.
Prior to 1999, the principal statutory responsibilities of UK NHS Trust Boards were to ensure proper financial management of the organisation and an acceptable level of patient safety. Trust Boards had no statutory duty to ensure a particular level of quality. Maintaining and improving the quality of care was understood to be the responsibility of the relevant clinical professions. As of 1999, Trust Boards assumed a legal responsibility for quality of care that is equal in measure to their other statutory duties. Clinical governance is the mechanism by which that responsibility is discharged.
"Clinical governance" does not mandate any particular structure, system or process for maintaining and improving the quality of care, except that designated responsibility for clinical governance must exist at Trust Board level, and that each Trust must prepare an Annual Review of Clinical Governance to report on quality of care and its maintenance. Beyond that, the Trust and its various clinical departments are obliged to interpret the principle of clinical governance into locally appropriate structures, processes, roles and responsibilities.
"Clinical Governance" is also one of the most frequently-occurring phrases in buzzword bingo
Buzzword bingo
Buzzword bingo is a bingo-style game where participants prepare bingo cards with buzzwords and tick them off when they are uttered during an event, such as a meeting or speech...
.
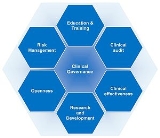
Elements of clinical governance

- Education and Training
- Clinical auditClinical auditClinical audit is a process that has been defined as "a quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change"....
- Clinical effectiveness
- Research and development
- Openness
- Risk management
- Information Management
Education and training
It is no longer considered acceptable for any clinician to abstain from continuing educationContinuing education
Continuing education is an all-encompassing term within a broad spectrum of post-secondary learning activities and programs. The term is used mainly in the United States and Canada...
after qualification - too much of what is learned during training becomes quickly outdated. In NHS
National Health Service
The National Health Service is the shared name of three of the four publicly funded healthcare systems in the United Kingdom. They provide a comprehensive range of health services, the vast majority of which are free at the point of use to residents of the United Kingdom...
Trusts, the continuing professional development of clinicians has been the responsibility of the Trust also been the professional duty of clinicians to remain up-to-date.
Clinical audit
Clinical audit is the review of clinical performance, the refining of clinical practice as a result and the measurement of performance against agreed standards - a cyclical process of improving the quality of clinical care. In one form or another, audit has been part of good clinical practice for generations. Whilst audit has been a requirement of NHSNational Health Service
The National Health Service is the shared name of three of the four publicly funded healthcare systems in the United Kingdom. They provide a comprehensive range of health services, the vast majority of which are free at the point of use to residents of the United Kingdom...
Trust employees, in primary care
Primary care
Primary care is the term for the health services by providers who act as the principal point of consultation for patients within a health care system...
clinical audit has only been encouraged, where audit time has had to compete with other priorities.
Clinical effectiveness
Clinical effectiveness is a measure of the extent to which a particular intervention works. The measure on its own is useful, but decisions are enhanced by considering additional factors, such as whether the intervention is appropriate and whether it represents value for money. In the modern health service, clinical practice needs to be refined in the light of emerging evidence of effectiveness but also has to consider aspects of efficiency and safety from the perspective of the individual patient and carers in the wider community.Research and development
Good professional practice has always sought to change in the light of evidence from research. The time lag for introducing such change can be very long and reducing time lag and associated morbidity requires emphasis not only on carrying out research, but also on using and implementing such research.Techniques such as critical appraisal
Critical appraisal
Critical appraisal is the use of explicit, transparent methods to assess the data in published research, applying the rules of evidence to factors such as internal validity, adherence to reporting standards, conclusions and generalizability. Critical appraisal methods form a central part of the...
of the literature, project management
Project management
Project management is the discipline of planning, organizing, securing, and managing resources to achieve specific goals. A project is a temporary endeavor with a defined beginning and end , undertaken to meet unique goals and objectives, typically to bring about beneficial change or added value...
and the development of guidelines, protocols
Clinical trial protocol
A clinical trial protocol is a document that describes the objective, design, methodology, statistical considerations, and organization of a clinical trial...
and implementation strategies are all tools for promoting the implementation of research practice.
Openness
Poor performance and poor practice can too often thrive behind closed doors. Processes which are open to public scrutiny, while respecting individual patient and practitioner confidentiality, and which can be justified openly, are an essential part of quality assurance. Open proceedings and discussion about clinical governance issues should be a feature of the framework.Any organisation providing high quality care has to show that it is meeting the needs of the population it serves. Health needs assessment and understanding the problems and aspirations of the community requires the cooperation between NHS
National Health Service
The National Health Service is the shared name of three of the four publicly funded healthcare systems in the United Kingdom. They provide a comprehensive range of health services, the vast majority of which are free at the point of use to residents of the United Kingdom...
organisations, public health departments, local authorities and community health councils.
The system of clinical governance brings together all the elements which seek to promote quality of care.
Risk management
Risk management involves consideration of the following components:Risks to patients: compliance with statutory regulations can help to minimise risks to patients. In addition, patient risks can be minimised by ensuring that systems are regularly reviewed and questioned - for example, by critical event audit and learning from complaints. Medical ethical standards
Medical ethics
Medical ethics is a system of moral principles that apply values and judgments to the practice of medicine. As a scholarly discipline, medical ethics encompasses its practical application in clinical settings as well as work on its history, philosophy, theology, and sociology.-History:Historically,...
are also a key factor in maintaining patient and public safety and well-being.
Risks to practitioners: ensuring that clinicians are immunised against infectious diseases, work in a safe environment and are helped to keep up-to-date are important parts of quality assurance.
Risks to the organisation: poor quality is a threat to any organisation. In addition to reducing risks to patients and practitioners, organisations need to reduce their own risks by ensuring high quality employment practice (including locum procedures and reviews of individual and team performance), a safe environment (including estates and privacy), and well designed policies on public involvement.
Information Management
Information Management in health:Patient records (demographic, Socioeconomic, Clinical information) proper collection, management and use of information within healthcare systems “will determine the system’s effectiveness in detecting health problems, defining priorities, identifying innovative solutions and allocating resources to improve health outcomes.
Applying clinical governance in the field
If clinical governance is to truly function effectively as a systematic approach to maintaining and improving the quality of patient care within a health system, it requires advocates. It also requires systems and people to be in place to promote and develop it.The system has found supporters outside of the UK. The not-for-profit UK hospital accreditation group the Trent Accreditation Scheme
Trent Accreditation Scheme
The Trent Accreditation Scheme , , was a British accreditation scheme formed with a mission to maintain and continually evaluate standards of quality, especially in health care delivery, through the surveying and accreditation of health care organisations, especially...
base their system upon NHS clinical governance, and apply it to hospitals in Hong Kong
Hong Kong
Hong Kong is one of two Special Administrative Regions of the People's Republic of China , the other being Macau. A city-state situated on China's south coast and enclosed by the Pearl River Delta and South China Sea, it is renowned for its expansive skyline and deep natural harbour...
and Malta
Malta
Malta , officially known as the Republic of Malta , is a Southern European country consisting of an archipelago situated in the centre of the Mediterranean, south of Sicily, east of Tunisia and north of Libya, with Gibraltar to the west and Alexandria to the east.Malta covers just over in...
.
External links
- UK NHS Clinical Governance Support Team
- Primary Care Training Centre
- Stephen BolsinStephen BolsinStephen Nicholas Cluley Bolsin is a British anaesthetist who became famous as the whistleblower whose actions to prevent incompetent paediatric cardiac surgery at the Bristol Royal Infirmary lead to the implementation of clinical governance reforms in the United Kingdom.- Career background...
- http://www.scribd.com/doc/9887146/Dody-Firmanda-Clinical-Leadership-Dan-Clinical-Governance-21-November-2007-KKI (Indonesian)
- http://www.scribd.com/doc/9881458/Dody-Firmanda-Clinical-Governance (Indonesian)

